药物性肝损伤(DILI)诊断:RUCAM量表与结构性专家诊断程序争鸣
2014-04-07 傅青春 中国医学论坛报
解放军第八五医院上海南京军区肝病中心 傅青春 来源:中国医学论坛报 2014年3月19-20日,美国食品与药物管理局(FDA)在华盛顿举办了第14届药物性肝损伤(DILI)专题研讨会。本报于上期(3月27日D1~D3)介绍FDA应对药物性肝损伤的策略、我国DILI研究进展和与国际水平的差距以及DILI研究新热点等,本期将继续推出大会精彩内容
解放军第八五医院上海南京军区肝病中心 傅青春 来源:中国医学论坛报

2014年3月19-20日,美国食品与药物管理局(FDA)在华盛顿举办了第14届药物性肝损伤(DILI)专题研讨会。本报于上期(3月27日D1~D3)介绍FDA应对药物性肝损伤的策略、我国DILI研究进展和与国际水平的差距以及DILI研究新热点等,本期将继续推出大会精彩内容,敬请关注。
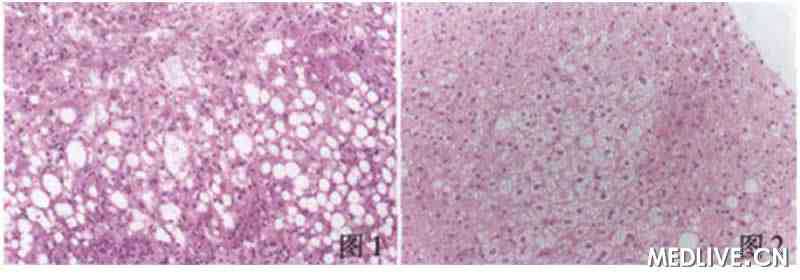
目前药物性肝损伤(DILI)的诊断没有明确的客观指标。在本届会议上,美国药物肝损伤研究网络(DILIN)专家委 员会的罗伯特?丰塔纳(Robert J.Fontana)教授认为,与因果关系评价量表(RUCAM)相比,结构性专家诊断程序(SEOP)更准确、可重复性强,是目前诊断DILI的最佳方 法,而英国诺丁汉大学艾萨尔(Aithal)则更信赖RUCAM,认为RUCAM作为一个相对客观的打分系统,在临床和科研中的价值远大于DILIN的专 家意见体系。正方观点SEOP是目前诊断DILI的最佳方法 美国DILIN专家委员会的共同主席Robert J.Fontana教授认为,DILI的诊断没有确认性的客观指标,临床诊断的主观性太强,相对客观的RUCAM量表已使用20余年,但因在酒精等多种参 数的定义上模棱两可、过度考虑再用药的权重、打分结果很低和不易使用等缺点,在临床上很少使用。
为此,2003年美国DILIN设计了一套结构性专家诊断程序(structured expert opinion process,SEOP),通过多达65页的临床试验观察表(CRF)收集完整的DILI诊断基本元素,由3名独立的肝病专家分别打分,帮助鉴别真正的DILI患者。
DILIN通过多中心前瞻性研究,直接比较了187例单药引起的可疑DILI SEOP和RUCAM因果评价表的报告,显示SEOP较RUCAM更可能形成DILI诊断。另外,3位独立评估者应用SEOP的初始评估完全一致率为 27%(50例/187例),评分相差在1分以内的概率为44%(83例/187例),因此SEOP评估法在总体上对70%病例的评判结果基本一致,而 RUCAM的初始评估完全一致率仅为19%。
SEOP的优势还包括对发病模式上的包容性,比如阿莫西林/克拉维酸导致的DILI往往停药后发生,呋喃妥因在长期用药后发生DILI; 可将病理和影像结果结合起来分析;可以参考LiverTox中的数据对多种药物引起的DILI患者进行相关药物排位和权重分配,对酒精性、缺血性、脓毒 症、胆石症和非酒精性脂肪性肝病等需要结合主观判断进行的鉴别诊断有优势。
因此,SEOP更准确、可重复性更强,是目前诊断DILI的最佳方法。其他团队的研究(如Hayashi)也证实了SEOP的总体可重复性好(κ=0.60),远高于RUCAM量表(κ=0.3441),因此有普适性,其缺点是不易推广。
美国南加州大学医学院DILIN专家唐?罗基(Don Rockey)教授是撰写SEOP与RUCAM量表对比的前瞻性研究论文的第一作者,其观点与Fontana教授一致。
Rockey教授曾报告1例新型头孢类抗生素引起DILI的女性患者,RUCAM量表评2分,SEOP判定高度可能,所以RUCAM量表 的结果不甚合理。这样的情况也出现在泰利霉素引起的DILI患者中,由于这部分患者的临床表现不典型,RUCAM量表的结果偏差较大,最后FDA采用 SEOP评估方法。
目前,美国DILIN正在积累可用的真实DILI病例,结合基因组学、生物标志、文献报道等方式,综合成基于网络的电子工具辅助DILI诊断,同时也在修订RUCAM量表的内容并电子化。反方观点在临床和科研中RUCAM价值远大于SEO
英国诺丁汉大学Aithal教授则更信赖RUCAM评分系统。其指出,人为犯错的概率通常超出人们的想象,据英国统计,早年由主治医师判断的DILI,经回顾分析其临床诊断正确率只有49%,英国黄卡系统报告的DILI中有47%不是DILI。
为尽可能克服专家观点的主观倾向,在欧洲诞生了RUCAM量表,其相对客观,独立专家的打分符合率84%(差别2分以内),明显不符合率 只有3%。经过适当训练的普通医生也能掌握RUCAM量表,但DILIN的SEOP则有一定难度,从事肝病专业的医生也不一定能掌握该体系的要求,更不用 说一般的内科医生。因此,作为一个相对客观的打分系统,在临床和科研中RUCAM量表的价值远大于DILIN的专家意见体系。
诺华公司科学家迈克尔?梅尔茨(Michael Merz)博士认为,虽然RUCAM量表有不少缺点,但相对合理客观、结构完整,不太难理解(适于非DILI专家用)、支持系统性数据收集,因此药物临床 试验中有其实用性。当然,RUCAM量表需要改进,比如参数和权重的抉择需要循证医学证据,填表指导要清楚完整。SEOP方法可作为不明确病例的进一步评 判工具。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CAM#
29
#结构性#
39
#肝损伤#
21
#损伤#
19
#DILI#
31
#药物性#
24