Stroke:丙戊酸钠减少蛛网膜下腔出血后的延迟脑损伤的研究
2016-12-30 MedSci MedSci原创
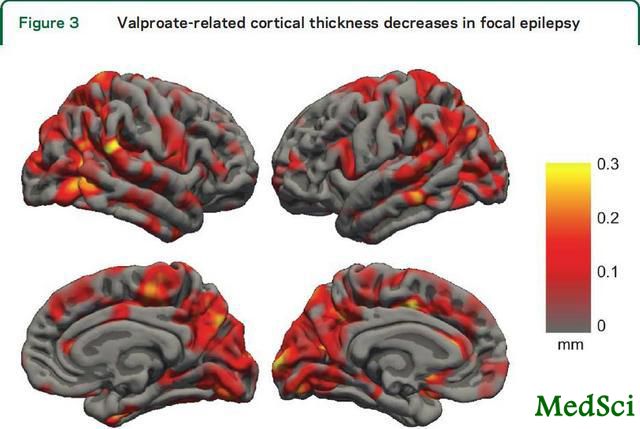
扩散性去极化(SD)可能导致蛛网膜下腔出血(SAH)后的迟发型脑缺血。近期,一项发表在STROKE杂志上的研究检测了SD的抑制剂丙戊酸钠是否减少SAH大鼠模型的大脑损伤。研究者们使用丙戊酸钠(200mg/kg)或载体预处理大鼠4周。通过右颈内动脉分叉血管内穿刺诱导大鼠SAH。建立SAH模型后一天,用T2-加权磁共振成像测量脑组织损伤,随后应用1mol/L KCl(诱导SDs)或NaCl(无SDs)
扩散性去极化(SD)可能导致蛛网膜下腔出血(SAH)后的迟发型脑缺血。近期,一项发表在STROKE杂志上的研究检测了SD的抑制剂丙戊酸钠是否减少SAH大鼠模型的大脑损伤。
研究者们使用丙戊酸钠(200mg/kg)或载体预处理大鼠4周。通过右颈内动脉分叉血管内穿刺诱导大鼠SAH。建立SAH模型后一天,用T2-加权磁共振成像测量脑组织损伤,随后应用1mol/L KCl(诱导SDs)或NaCl(无SDs)。在第3天重复磁共振成像检查,随后通过组织学检查确认神经元死亡。神经功能使用倾斜斜率试验评估。
此项研究结果显示,在使用KCl的大鼠组中,丙戊酸钠处理的第1天和第3天之间的损伤生长为57±73mm3,而在载体处理组中为237±232mm3。
在无SD诱导的组中,丙戊酸钠和载体处理组中的损伤生长分别为8±20mm3及27±52mm3。
在拟合方差模型的双向分析中,研究者们发现治疗组和KCl/NaCl应用组之间有显着的相互作用效应(P = 0.04)。SDs的数量和持续时间、死亡率和神经功能在两组之间没有显著的统计学差异。
磁共振成像上的损伤生长与组织学梗死体积相关(Spearman's rho=0.83;P=0.0004),与原发性损害相比,损伤生长区域的神经元死亡减少。
此项研究得出结论:在大鼠SAH模型中,丙戊酸钠治疗显着减少KCl应用后的脑损伤。
原始出处:
Hamming AM, van der Toorn A, Rudrapatna US, Ma L, van Os HJ, Ferrari MD, van den Maagdenberg AM, van Zwet E, Poinsatte K, Stowe AM, Dijkhuizen RM, Wermer MJ. Valproate Reduces Delayed Brain Injury in a Rat Model of Subarachnoid Hemorrhage. Stroke. 2016 Dec 27. pii: STROKEAHA.116.014738. doi: 10.1161/STROKEAHA.116.014738.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#蛛网膜#
40
#损伤#
26
#丙戊酸#
36
#丙戊酸钠#
39