ESC Heart Failure:更年期与心力衰竭之间的关系
2021-06-29 MedSci原创 MedSci原创
心力衰竭已成为全球健康问题,影响着全世界约 2600 万人,尤其对64 岁以上的患者。有研究显示,老年心力衰竭女性比男性面临更大的风险,绝经后女性发生射血分数保留的心力衰竭 (HFpEF) 的患病率明
心力衰竭已成为全球健康问题,影响着全世界约 2600 万人,尤其对64 岁以上的患者。有研究显示,老年心力衰竭女性比男性面临更大的风险,绝经后女性发生射血分数保留的心力衰竭 (HFpEF) 的患病率明显更高。然而,由于缺乏有效的 HFpEF 循证治疗,在管理HFpEF上具有挑战性,

pixabay
大多数HFpEF 的治疗都针对危险因素和合并症,包括高血压、糖尿病和肥胖症等。但与男性相比,更年期可能是女性特有的特异性风险因素。先前有研究表明,更年期的女性冠心病发生风险显著增加。那么,更年期是否可以预测心力衰竭事件或可能的合并症可归因的风险负担。
近日,发表在ESC Heart Failure一项研究探讨更年期与心力衰竭之间的关系。结果发现,更年期女性与患冠心病风险相关,但与心力衰竭发生风险无关。

在这项研究中,研究人员纳入了来自台湾健康保险数据库中14340名更年期女性作为实验组,且这些女性没有冠心病或心力衰竭病史。同时,纳入了14340名与之相匹配的女性作为对照组。研究人员调查了心力衰竭可能的合并症归因风险,并评估了更年期是否在心力衰竭风险中起作用。
研究结果显示,实验组心力衰竭发病率并没有明显低于对照组(每1000人年4.87 vs. 5.06,P = 0.336),且合并症负担较重的女性患心力衰竭和冠心病的风险按比例增加。与实验组相比,风险因素负担对对照组的心力衰竭风险影响更大(≥5 个风险因素,调整后的风险比为 25.69 vs. 14.75)。

实验组和对照组心力衰竭累积发生率
无论是否是更年期,接受激素治疗的女性患心力衰竭的风险没有明显影响。亚组分析显示,与对照组相比,实验组患心力衰竭风险在所有亚组中均未显著增加。
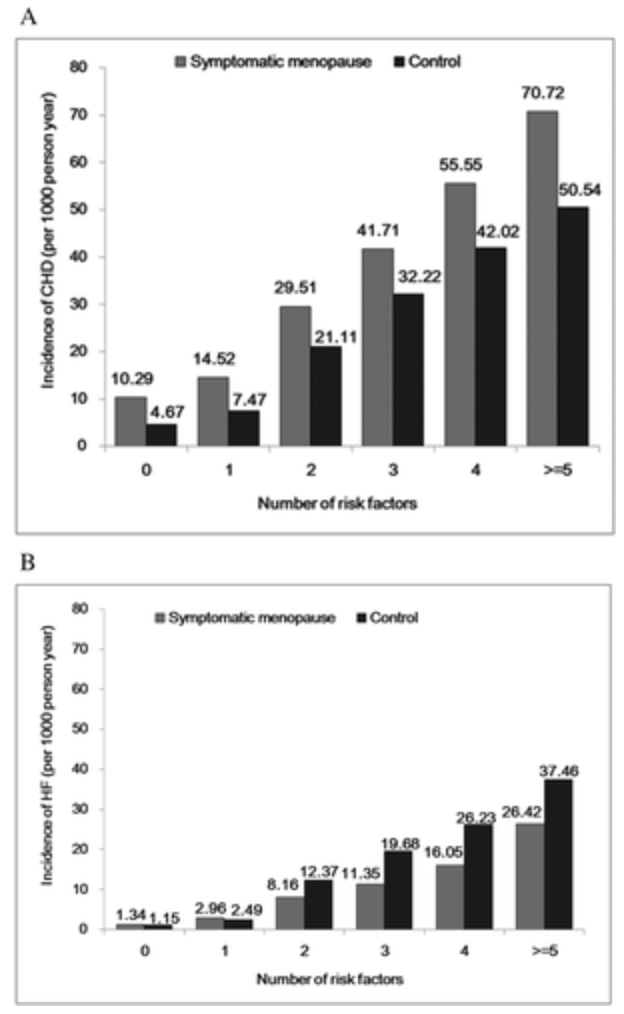
实验组和对照组危险因素数量与冠心病(A)或 心力衰竭(B)发生率之间的关系
综上,这项大规模纵向回顾性队列研究显示,更年期与冠心病发生风险相关,但与心衰无关。传统风险因素而非更年期在女性心衰风险中起着重要作用。
原始出处
黄清辉, Chew-Teng Kor , Ie-Bin Lian , Chia-Chu Chang.Menopausal symptoms and risk of heart failure: a retrospective analysis from Taiwan National Health Insurance Database. ESC Heart Failure.20 June 2021 https://doi.org/10.1002/ehf2.13480
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#failure#
30
#ART#
30
#HEART#
35
好
53