Cell:挑战常规!先天性免疫系统经训练后随时准备应对未来的危险
2018-01-16 佚名 “细胞”微信号
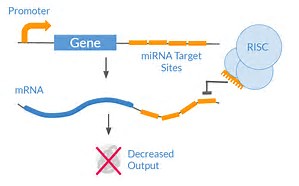
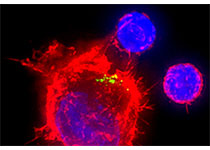
当你接种抵抗脊髓灰质炎或流感等疾病的疫苗时,你的免疫系统会加速抵御这种特定的感染。但是,如果你感染了水痘病毒,或者甚至感染了一种略微不同的流感病毒毒株,那么你的运气就不好了。这是因为传统的疫苗努力激活适应性免疫系统。适应性免疫系统的功能主要由高度特异性的靶向特定威胁的T细胞和B细胞执行。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
25
#CEL#
24
好资源
62
好资源
67
好资源
62
好资源
44
好资源
62
好资源
20
好资源
25
好资源
22