Aging Cell: 肿瘤抑制因子miR-34c作为AD治疗新靶点
2022-08-31 brainnew神内神外 brainnews白色世界 发表于上海
解密阿尔茨海默病和肿瘤发生负相关的分子机理
流行病学研究表明,阿尔茨海默病(AD)与癌症之间存在负相关性,河北医科大学徐顺江教授团队因此关注到肿瘤抑制因子miR-34c的上游信号通路和下游分子机制在AD病理中起着关键作用,在Aging Cell上发表题为Increased miR‐34c mediates synaptic deficits by targeting synaptotagmin 1 through ROS‐JNK‐p53 pathway in Alzheimer’s Disease的文章,讲述通过ROS-JNK-p53途径和miR-34c/SYT1途径可靶向SYT1,增加miR-34c介导的突触和记忆缺陷,被认为是AD患者新的治疗靶点。
1miR-34c受ROC-JNK-p53调控,且与AD病理相关
本研究首先在体内(SAMP8小鼠模型-衰老加速模型)及体外(H2O2刺激的氧化应激神经元和Aβ42刺激的AD细胞模型)确定miR-34c的表达水平增加。结果发现ROS产生、JNK激活、p53积累参与SAMP8小鼠海马神经元损伤,这表明ROS-JNK-p53通路参与AD病理过程。本研究进一步验证氧化应激诱导的miR-34c的增加是由ROS-JNK-p53途径介导。
2miR-34c靶向调节SYT1
生物信息学分析预测miR-34c的靶基因,并进行验证。结果显示miR-34c直接结合SYT1 mRNA序列的3'-UTR,同时表明miR-34c在神经元中SYT1(突触前神经末梢释放神经递质中起关键作用)表达的转录后调节中起功能性作用,并在小鼠模型中得到验证。以上结果证实了ROS-JNK-p53途径和miR-34c/SYT1途径在AD中的分子机制。接着通过SAMP8小鼠模型表明SM34c抑制miR-34c可减轻Aβ诱导的突触衰竭,改善认知缺陷。
3轻度认知障碍(aMCI)患者血清miR-34c水平升高
aMCI是正常衰老和痴呆之间的过渡阶段,代表AD的早期阶段。临床实验证实aMCI患者miR-34c血清水平升高,且与MMSE评分呈正相关。进一步使用ROC曲线评估miR-34c对aMCI诊断价值,结果显示循环miR-34c可能是诊断的预测生物标志物。
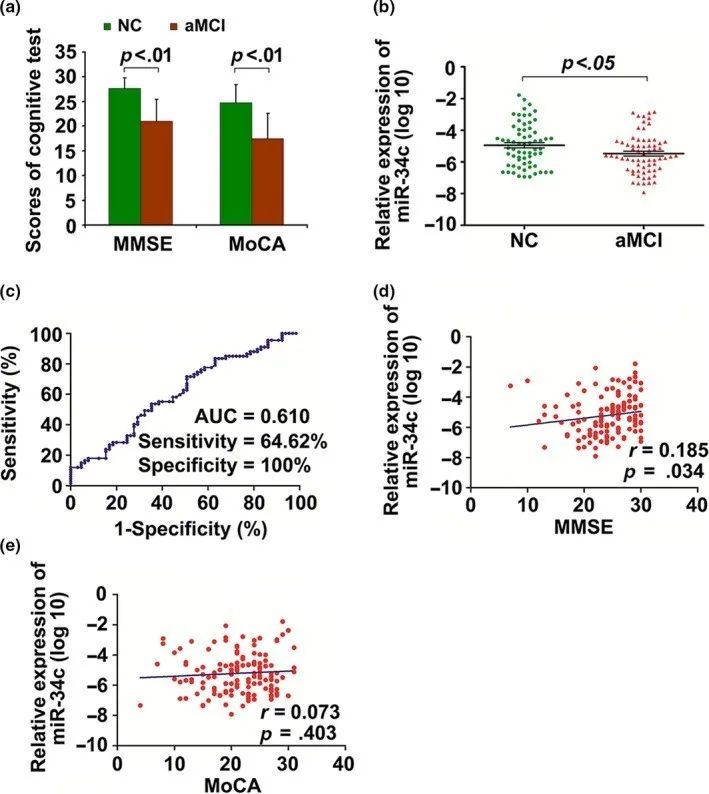
图. aMCI患者血清miR-34c表达水平升高
AD是与衰老相关的疾病,关键病理学标志之一为Aβ的异常积累,会导致突触丧失、神经元死亡和记忆缺陷,而海马突触可塑性的下降是AD的早期事件。癌症是老年人中普遍存在的另一种疾病,其特征是细胞增殖的不受控。一些流行病学报告AD与癌症之间存在负相关。本文从细胞途径和分子机制的角度探讨肿瘤抑制因子在AD中的作用,将有助于开辟针对这两种疾病的预防和治疗新领域。
编译作者:小飞侠 (Brainnews创作团队)
校审:Victoria, Simon (Brainnews编辑部)
参考文献:
Shi Z, Zhang K, Zhou H, et al. Increased miR-34c mediates synaptic deficits by targeting synaptotagmin 1 through ROS-JNK-p53 pathway in Alzheimer's Disease. Aging Cell. 2020;19(3):e13125. doi:10.1111/acel.13125
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#miR#
45
#Cell#
28
#肿瘤抑制因子#
39
#肿瘤抑制#
41
#CEL#
30
#新靶点#
0
#治疗新靶点#
45
#抑制因子#
34