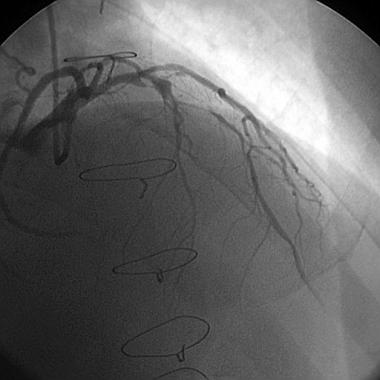
支架内再狭窄(图)和支架术后再狭窄(图)
2015-12-02 网络 MedSci原创
支架置入术是目前治疗冠心病的最主要的治疗方法,虽然药物支架的出现明显降低了支架再狭窄的发生率,但是并没有消除支架再狭窄。因此,随着支架置入患者数的增加,再狭窄患者也逐渐增多。然而再狭窄病变如果再次放支架,由于金属套金属再狭窄几率高很多。近年来,出现的药物球囊是治疗再狭窄病变的一种选择,药物球囊的意思是球囊表面带防止再狭窄的药物,在再狭窄病变充分扩张后应用药物球囊将药物释放到病变部位,再将球囊退
支架置入术是目前治疗冠心病的最主要的治疗方法,虽然药物支架的出现明显降低了支架再狭窄的发生率,但是并没有消除支架再狭窄。因此,随着支架置入患者数的增加,再狭窄患者也逐渐增多。然而再狭窄病变如果再次放支架,由于金属套金属再狭窄几率高很多。近年来,出现的药物球囊是治疗再狭窄病变的一种选择,药物球囊的意思是球囊表面带防止再狭窄的药物,在再狭窄病变充分扩张后应用药物球囊将药物释放到病变部位,再将球囊退回,在避免再狭窄的同时避免了再次置入支架。在国外的研究当中已经证实了药物球囊的疗效,在PEPCADII ISR试验中,比较应用药物球囊和再次置入支架后发生再狭窄的几率在药物球囊中为7%,而在支架组为20%。虽然药物球囊也不能100%避免再狭窄的发生,但是对部分患者减少了体内支架套支架的几率。目前国内药物球囊仅是临床试验阶段,我们医院也是参加单位,估计不久的将来会在我国上市应用,给患者带来一种新的治疗选择。

支架内再狭窄

支架术后再狭窄
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#支架术#
38
#支架内再狭窄#
29
#支架术后#
0
#再狭窄#
37