EUR J Cancer:化疗联合塞来昔布或曲妥珠单抗治疗乳腺癌患者的多中心随机II期临床试验
2017-12-30 MedSci MedSci原创
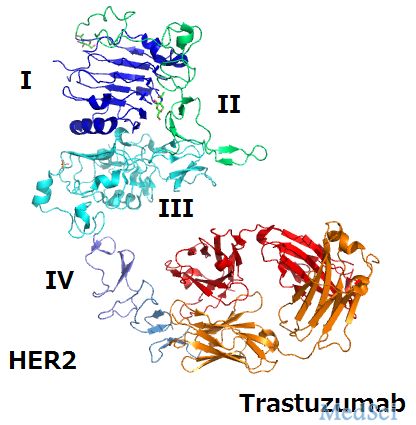
一项多中心随机II期试验显示,新辅助化疗(NAC)联合曲妥珠单抗相比于新辅助化疗(NAC)联合塞来昔布在治疗HER2阳性乳腺癌患者过程中能够显著增加病理完全反应率(pCR)。根据这项临床试验,研究者们报道了无病生存期(DFS)和总生存期(OS)的长期随访结果。
一项多中心随机II期试验显示,新辅助化疗(NAC)联合曲妥珠单抗相比于新辅助化疗(NAC)联合塞来昔布在治疗HER2阳性乳腺癌患者过程中能够显著增加病理完全反应率(pCR)。根据这项临床试验,研究者们报道了无病生存期(DFS)和总生存期(OS)的长期随访结果。
从2004年到2007年,340例乳腺癌患者被随机分配接受新辅助化疗(四个周期的表柔比星/环磷酰胺 + 四个周期的多西他赛),其中新辅助化疗联合塞来昔布的病例数为220例,新辅助化疗联合曲妥珠单抗的病例数为120例。
结果显示,在长达8年的随访中(94.4个月),在HER2阴性亚组中塞来昔步与DFS获益无关。在HER2阳性群体中,新辅助化疗联合曲妥珠单抗与DFS获益无关。值得注意的是,相比于HER2阴性的乳腺癌患者,DFS和OS在HER2阳性患者中显著较高(HR=0.58,95% CI 0.36-0.92,p=0.021)。
因此,新型辅助化疗联合塞来昔布不能为HER2阴性患者带来生存获益。曲妥珠单抗的引入显著增加病理完全反应率(pCR),但对DFS和OS没有影响。
原始出处:
Giacchetti,
Sylvie, et al. "Long-term outcome of the REMAGUS 02 trial, a multicenter
randomised phase II trial in locally advanced breast cancer patients treated with
neoadjuvant chemotherapy with or without celecoxib or trastuzumab according to
HER2 status." European Journal of Cancer 2017 75: 323-332. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#曲妥珠#
0
#多中心#
27
#II期临床试验#
23
#I期临床试验#
22
#I期临床#
33
#塞来昔布#
41
#II期临床#
24
#乳腺癌患者#
20