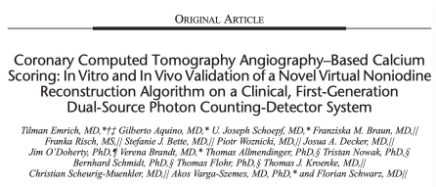
Investigative Radiology:临床第一代双源光子计数CT系统在CCTA钙化评分方面的价值
2022-09-09 shaosai MedSci原创
近,光子计数探测器计算机断层扫描(PCD-CT)扫描仪已引入临床。除了更高的空间分辨率和更高的剂量效率,PCD-CT数据集包含可用于多物质分解的差异化光谱信息。
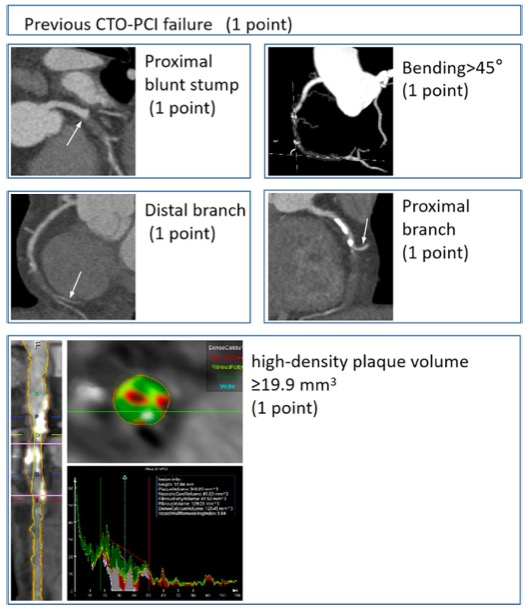
现阶段,冠状动脉钙化评分(CACS)是对有症状和无症状患者进行风险评估的重要方法之一。随着CACS的风险评估,冠状动脉计算机断层扫描(CCTA)已被确立为评估冠状动脉疾病(CAD)存在和程度的一线检查。随着双能量和光谱成像技术的出现,一些算法允许从CCTA数据集的虚拟非对比(VNC)图像中评估CACS,使用材料分解为2种材料(软组织和碘)。由于钙既不是由碘也不是由软组织表示,所有上述使用双能量技术的方法都显示出高相关性,但对来自虚拟非增强图像的冠状动脉钙(CAC)评分有相关的低估。
最近,光子计数探测器计算机断层扫描(PCD-CT)扫描仪已引入临床。除了更高的空间分辨率和更高的剂量效率,PCD-CT数据集包含可用于多物质分解的差异化光谱信息。
近日,发表在Investigative Radiology杂志的一项研究在第一代双源PCD-CT系统上使用CCTA数据集的PureCalcium重建来评估CACS,并与VNC重建和TNC采集的CACS在模型和患者群体中进行了比较,为临床提供了一个更准确的重建技术。
尽管CACS和CCTA是评估冠状动脉疾病的成熟技术,但两者为互补性的采集方法,会增加的扫描时间和病人辐射剂量。因此,从一次CCTA采集中得到准确的CACS是非常可取的。本项研究中基于PureCalcium、VNC和TNC重建的CACS是在一个CACS模型和67名接受CCTA的患者(70[59/80]岁,58.2%为男性)中进行的评估,这些患者均在第一代光子计数探测器-计算机断层扫描系统上接受了CCTA检查。对3种重建的冠状动脉钙质评分进行了量化,并使用Wilcoxon测试进行比较。通过Pearson和Spearman相关性和Bland-Altman分析来评估一致性。使用Cohen κ对冠状动脉钙质评分类别(0、1-10、11-100、101-400和>400)进行了比较。
模型研究显示CACSPureCalcium和CACSTNC之间有很强的一致性(60.7±90.6 vs 67.3±88.3,P=0.01,r=0.98,类内相关[ICC]=0.98)。 而CACSVNC显示出明显的低估(42.4 ± 75.3 vs 67.3 ± 88.3,P < 0.001,r = 0.94,ICC = 0.89;平均偏差,24.9;LoA,-87.1/37.2)。体内比较证实了高度的相关性,但显示了CACSPureCalcium的低估(169.3 [0.7/969.4] vs 232.2 [26.5/1112.2],P < 0.001,r = 0.97,ICC = 0.98;平均偏差,-113.5;LoA,-470.2/243.2)。相比之下,CACSVNC显示出类似的高相关性,但低估程度大得多(24.3 [0/272.3] vs 232.2 [26.5/1112.2],P < 0.001,r = 0.97,ICC = 0.54;平均偏差,-551.6;LoA,-2037.5/934.4)。CACSPureCalcium显示CACS分类的一致性(κ = 0.88)优于CACSVNC(κ = 0.60)。
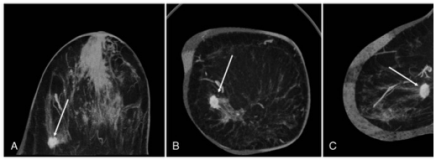
图 69岁男性患者的图像示例,LAD有钙化。TNC(A)和VNI(B)与CAC评分模块的颜色重叠。VNI低估了LAD的钙化量。TNC CACS总数=1633;VNI CACS=1391
本研究表明,基于CCTA的PureCalcium重建的CACS定量和分类的准确性优于来自VNC重建的CACS,可实现临床上辐射剂量的优化和采集时间高效的CAD综合评估。
原文出处:
Tilman Emrich,Gilberto Aquino,U Joseph Schoepf,et al.Coronary Computed Tomography Angiography-Based Calcium Scoring: In Vitro and In Vivo Validation of a Novel Virtual Noniodine Reconstruction Algorithm on a Clinical, First-Generation Dual-Source Photon Counting-Detector SystemCoronary Computed Tomography Angiography-Based Calcium Scoring: In Vitro and In Vivo Validation of a Novel Virtual Noniodine Reconstruction Algorithm on a Clinical, First-Generation Dual-Source Photon Counting-Detector System.DOI:10.1097/RLI.0000000000000868
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CCT#
43
#第一代#
37
#CTA#
46
#EST#
27
#IgA#
45