Clin Cancer Res:肿瘤浸润B细胞可预测采用达拉非尼+曲美替尼治疗的黑色素瘤患者的临床预后
2021-08-16 Nebula MedSci原创
B 细胞可作为潜在的生物标志物,来预测接受达拉非尼联合曲美替尼治疗的晚期黑色素瘤患者的临床预后
虽然不可切除或转移性黑色素瘤患者使用 BRAF 和 MEK 靶向药物或免疫检查点抑制剂可治疗的长期生存期可超过 5 年,但大部分患者会出现耐药性。目前缺乏可确定哪些患者能从各种类型治疗中获益的生物标志物。大多数研究集中于 T 细胞在抗肿瘤反应中的预测作用上,对 B 细胞的关注甚少。
Brase等研究人员采用基因表达谱和数字病理学,对146例既往未治疗过的携带BRAF v600 突变的转移性黑色素瘤患者进行了预定的探索性生物标志物分析,这些患者来自随机化的III期COMBI-v试验,接受了达拉非尼+曲美替尼治疗,并留有可用的肿瘤样本。
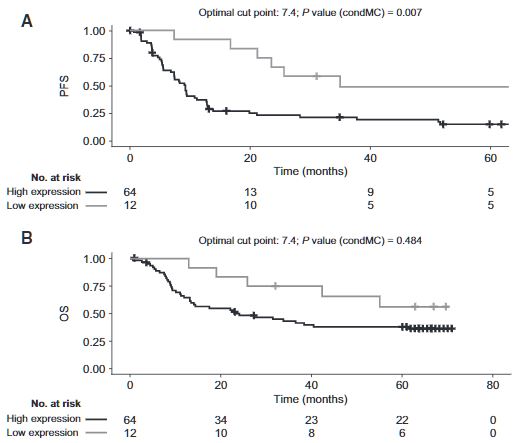
根据B细胞基因特征分组的患者的PFS和OS
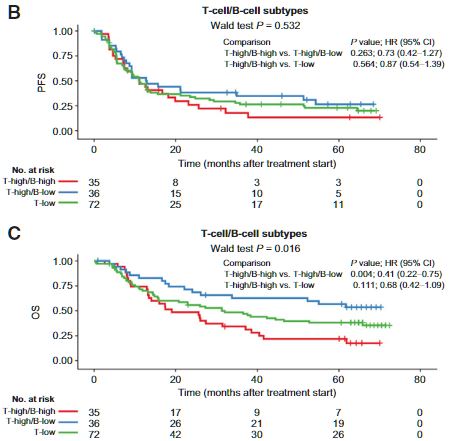
基线细胞周期基因表达特征与无进展生存期相关(p=0.007)。与具有高 T 细胞/高 B 细胞基因特征的患者相比,具有高 T 细胞/低 B 细胞基因特征的患者的中位总生存期有所延长(未达到 [95%CI 33.8-未达到] vs 19.1个月 [95%CI 13.4-38.6])。具有高 B 细胞特征的患者在肿瘤区室中具有高水平的 B 细胞浸润,这与 MAPK 活性降低和免疫抑制标志物表达增加相对应。
根据T细胞和B细胞浸润水平分组的患者的PFS和OS
综上所述,B 细胞可作为潜在的生物标志物,来预测接受达拉非尼联合曲美替尼治疗的晚期黑色素瘤患者的临床预后。鉴于单独的研究表明 B 细胞水平和对免疫疗法的反应有相反的效应,B 细胞可以作为促进治疗选择的潜在生物标志物。需要在更大规模的患者队列中进一步验证该研究结果。
原始出处:
Jan C. Brase, et al. Role of Tumor-Infiltrating B Cells in Clinical Outcome of Patients with Melanoma Treated With Dabrafenib Plus Trametinib. Clin Cancer Res August 15 2021 27 (16) 4500-4510; DOI:10.1158/1078-0432.CCR-20-3586
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#色素#
34
#B细胞#
41
#达拉非尼#
36
#临床预后#
37
#黑色素#
31
#黑色素#
25
很有意思的研究
67