JACC:外科主动脉瓣置换术的远期预后研究
2018-03-27 MedSci MedSci原创
本研究的目的旨在评估接受外科主动脉瓣置换术(SAVR)患者的远期临床预后和瓣膜的结构退化(SVD)情况。本研究纳入了2002年至2004年接受SAVR治疗的672名(平均年龄72 ± 8岁,男性占61.5%)患者,其中对624名术后出院的患者进行了心超检查,在术后随访10年后对209名患者进行了心超检查。经过平均10年时间的随访,432名(64.3%)患者出现了死亡。高龄、左室功能不良、房颤、慢性
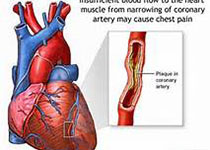
本研究的目的旨在评估接受外科主动脉瓣置换术(SAVR)患者的远期临床预后和瓣膜的结构退化(SVD)情况。本研究纳入了2002年至2004年接受SAVR治疗的672名(平均年龄72 ± 8岁,男性占61.5%)患者,其中对624名术后出院的患者进行了心超检查,在术后随访10年后对209名患者进行了心超检查。经过平均10年时间的随访,432名(64.3%)患者出现了死亡。高龄、左室功能不良、房颤、慢性阻塞性肺疾病、高体质指数和糖尿病与高的死亡风险呈相关性(p<0.05)。有6.6%的患者出现有SVD事件,30.1%的患者出现有亚临床SVD事件。高的体质指数和主动脉瓣假体植入与SVD事件的发生呈相关性,其中83%的患者再次接受了主动脉瓣手术干预。研究结果显示,接受外科主动脉瓣置换术治疗患者的10年死亡率较高,主要与高龄和并发症的发生相关。原始出处:Tania R et al.Long-Term Outcomes Following Surgical Aortic Bioprosthesis Implantation.JACC.2018 Apr.本文系梅斯医学(MedSci)原创编译整理
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#外科主动脉瓣置换术#
39
#JACC#
34
#置换#
24
#远期预后#
38
这里说的是生物瓣.
67
#ACC#
27
#主动脉瓣#
26
#主动脉瓣置换术#
24
#主动脉#
28
#置换术#
29