Cancer Cell & Nat Med:喜人!新药可能对急性白血病和前列腺癌有效
2015-03-31 Zhang JL译 MedSci原创
来自密歇根大学综合癌症中心的研究人员在实验室研究中开发出一种能够治疗一种罕见类型的急性白血病的新药。另外的研究显示相同的化合物可能在前列腺癌的治疗中发挥作用。该复合物是由Jolanta Grembecka博士和Tomasz Cierpicki博士的实验室所开发的。该实验室在过去的多年研究中,主力研发一种小分子抑制剂,以阻止蛋白质menin和MLL融合蛋白之间相互作用,而后者则是导致一种罕见的急性白
来自密歇根大学综合癌症中心的研究人员在实验室研究中开发出一种能够治疗一种罕见类型的急性白血病的新药。另外的研究显示相同的化合物可能在前列腺癌的治疗中发挥作用。
该复合物是由Jolanta Grembecka博士和Tomasz Cierpicki博士的实验室所开发的。该实验室在过去的多年研究中,主力研发一种小分子抑制剂,以阻止蛋白质menin和MLL融合蛋白之间相互作用,而后者则是导致一种罕见的急性白血病发病的主要原因。
所谓MLL融合白血病可能发生在成年人和儿童中。它占的成人急性白血病10%,以及婴儿急性白血病的大约70%。目前的治疗不是非常有效,仅有大约三分之一的病人能够存活5年。
蛋白质-蛋白质之间的关系如menin-MLL融合蛋白质的相互作用在白血病中通常被认为是“无法解开”,这意味着开发靶向这种蛋白间相互作用的药物具有相当大的挑战性。然而,Grembecka认为,尽管困难重重,研究MLL与menin的相互作用依然具有一定前景。
“在许多类型的癌症中,你可以看到多种相互作用和突变,导致癌症的发生。MLL-menin相互作用是一个很好的药物靶点,因为它是这种类型白血病的主要成因。通过阻断这种相互作用,很可能会阻止癌症的发生发展。” 密歇根大学医学院病理学助理教授Grembecka说。
在Cancer Cell发表的一项研究中,研究者们在MLL白血病细胞系和小鼠中测试了他们所开发了两种化合物,mi-463和mi-503。他们发现这些化合物能够阻止MLL-menin的相互作用而不损害正常的血细胞。化合物在血液中的输送和代谢率好,这两个均是开发新药物的关键问题。
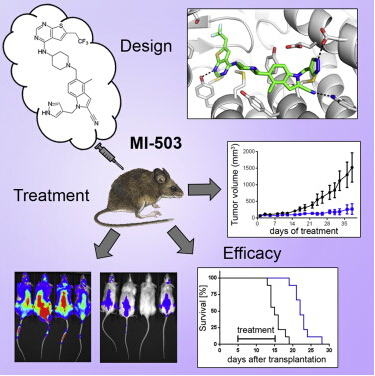
研究人员先前对上一个版本的化合物进行了测试,效果喜人。在本项研究中,他们大大提高了药物的效力和它的许多药物性质,使其更有在人类身上使用的潜在能力。
密歇根大学医学院病理学助理教授Cierpicki说:“尽管困难重重,我们决定探索寻找一种方法来通过应用小分子化合物来阻止MLL-menin的相互作用。从无到有,我们已经能够识别并大大提高这种化合物,并且结果表明它在动物模型中有潜在阻断MLL融合白血病的能力。”。
与此同时,密歇根大学的研究人员发现,menin与MLL在前列腺癌雄激素受体信号中发挥重要作用,而后者则是前列腺癌的一个关键驱动因素。在发表在Nature Medicine的一项研究中,研究人员应用相同MLL-menin抑制剂对前列腺癌去势抵抗细胞和小鼠模型进行了测试。
该篇Nature Medicine 研究的作者、密歇根转化临床病理中心的主任Arul M. Chinnaiyan博士表示:“我们的研究表明,这种MLL-menin抑制剂也可能对更常见的固体肿瘤有潜在作用,比如前列腺癌。”
进行进一步临床试验之前,这种化合物必须在实验室经过更多的测试和分析。Grembecka 和Cierpicki的实验室正在对他们的抑制剂进一步细化研究和进行更深入的测试。Chinnaiyan的团队将继续调查MLL在去势抵抗的前列腺癌中的作用。
原始出处:
Jolanta Grembecka et al. Pharmacologic inhibition of the menin-MLL interaction blocks progression of MLL leukemia in vivo. Cancer Cell, March 2015 DOI: 10.1016/j.ccell.2015.02.016
Rohit Malik, Amjad P. Khan, Irfan sA. Asangani, Marcin Cieslik, John R. Prensner, Xiaoju Wang, Matthew K. Iyer, Xia Jiang, Dmitry Borkin, June Escara-Wilke, Rachell Stender, Yi-Mi Wu, Yashar S. Niknafs, Xiaojun Jing, Yuanyuan Qiao, Nallasivam Palanisamy, Lakshmi P. Kunju, Pranathi M. Krishnamurthy, Anastasia K. Yocum, Dattatreya Mellacheruvu, Alexey I. Nesvizhskii, Xuhong Cao, Saravana M. Dhanasekaran, Felix Y. Feng. Targeting the MLL complex in castration resistant prostate cancer. Nature Medicine, March 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
25
#Nat#
30
#CEL#
31
不错,学习了
116
#cancer cell#
29
#Med#
18
有意义
111