Arch Med Res :降低 COVID-19 门诊患者住院/死亡风险的多模式策略
2022-03-06 从医路漫漫 MedSci原创
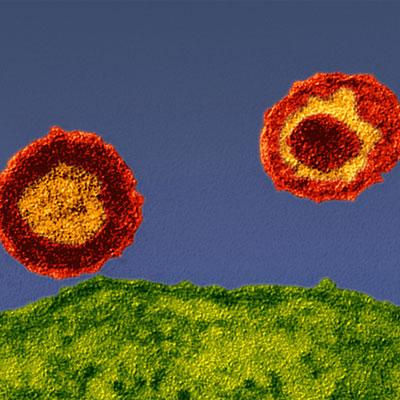
自2020年3月开始以来,COVID-19(2019 年冠状病毒病)的广泛传播已达到前所未有的大流行比例

背景:自2020年3月开始以来,COVID-19(2019 年冠状病毒病)的广泛传播已达到前所未有的大流行比例,确诊病例已超过2.7亿,死亡人数超过500万受到COVID-19 的打击,不仅面临历史性的医学挑战,还面临大流行的社会和经济后果。因此,及时识别可以在家远程管理的患者对于减轻医院负担至关重要,使他们能够专注于重症患者的护理。大多数感染新型SARS-CoV -2病毒(严重急性呼吸综合征冠状病毒的人呈现出一种相当温和的疾病形式,可以在家中通过一般支持性护理轻松控制。然而,不同比例的患者会发展为更严重的感染形式,从轻度需氧间质性肺炎到伴有多器官衰竭的破坏性呼吸窘迫综合征,因此需要住院甚至重症监护病房以提供侵入性治疗。机械通气和血流动力学支持。跟踪COVID-19 患者的远程医疗策略包括电话或视频通话、智能手机应用程序、基于人工智能技术的机器人呼叫。和家庭患者单元实时监测血氧饱和度、心率、体温和呼气峰值流量等临床参数。世界各地已实施了不同的干预措施,对轻度COVID-19患者进行家庭监测,以减轻医疗保健系统的负担并保证护理质量。电话随访和治疗包尚未在全国初级保健计划的背景下进行评估。
研究目的:比较发展中国家接受和未接受治疗包和电话随访的门诊患者因 COVID-19 住院和死亡的风险。使用来自墨西哥社会保障研究所医疗信息系统的数据进行了两组比较分析。我们总共纳入了 28,048 名实验室确诊的 SARS-CoV -2 患者:7,898 名(28.2%)接受了医疗包,20,150 名(71.8%)没有接受。计算住院和死亡发生率。为了确定住院或死亡与治疗医疗包之间的显着关联,我们使用多变量逻辑模型计算了风险比。
结果。接受试剂盒的患者住院率为 6.14%,未接受试剂盒的患者住院率为 11.71%。男性、年龄和肥胖、高血压、糖尿病、免疫抑制或肾脏疾病病史与住院或死亡风险增加相关。接受医疗包或电话随访的患者的风险率降低。在多变量模型中,接受医疗包与较低的 COVID-19 住院或死亡风险相关:调整后的风险比为 0.41(95% 置信区间为 0.36-0.47)。
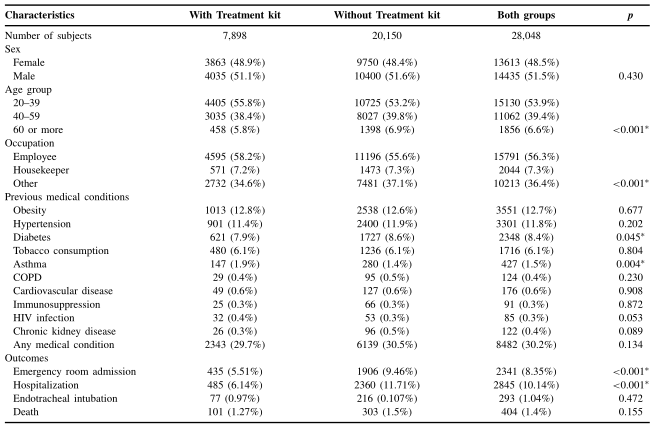
表 1. 评估住院或死亡相对风险的单变量和多变量分析
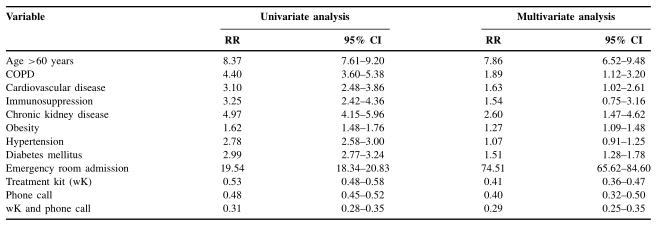
表2. 评估住院或死亡相对风险的单变量和多变量分析
结论。使用多模式策略可能会降低轻度 COVID-19 成人门诊患者的住院和死亡风险。
原文出处:Ascencio-Montiel IJ, Tomás-López JC, Álvarez-Medina V, et al.A Multimodal Strategy to Reduce the Risk of Hospitalization/death in Ambulatory Patients with COVID-19.Arch Med Res 2022 Jan 24
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#门诊患者#
36
学习学习
53
好的研究方向……
48
#死亡风险#
28
#Med#
27