JACC:经皮室间隔消融术治疗肥厚型梗阻性心肌病安全有效
2018-10-11 MedSci MedSci原创
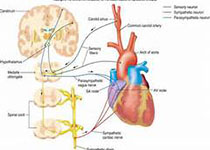
对于由肥厚型梗阻性心肌病(HOCM)致残的患者,经皮心肌内间隔射频消融术(PIMSRA)可能是一个侵入性低的治疗选择。本研究的目的旨在评估PIMSRA对缓解HOCM患者的左室流出道压差的安全性和有效性。本研究纳入了15例HOCM患者,并在术后6个月的随访期间对其心电图、影像学和生化检测进行评估。经过6个月时间的随访,患者的左室流出道峰值压差明显降低(静息压差88.00 [66.00] mm Hg
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#室间隔#
48
#JACC#
45
#ACC#
0
#消融#
51
#消融术#
40
#消融术#
36
#肌病#
32
学习了
61