科学家研发用于治疗年龄相关性黄斑变性的眼药水 有望取代注射治疗
2017-05-17 cnBeta cnBeta
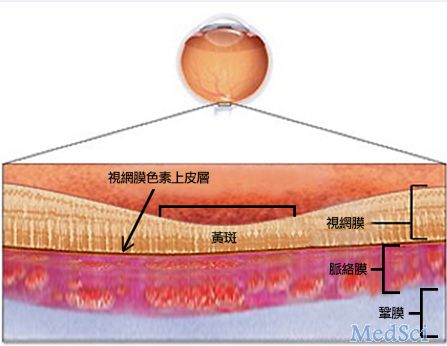
年龄相关性黄斑变性 (AMD) 是一种导致老年人致盲的常见疾病,是一种可引起视力迅速丧失的视网膜退行性病变。患者每月需要用注射液进行治疗。 据外媒报道,现在伯明翰大学的科学家团队开发了一种突破性的新治疗方法,用简单的眼药水可取代此前的注射液。据悉,仅在英国,AMD 就影响了超过 60 万人。而在美国,这种疾病是 50 岁以上人群失明的最常见原因之一。目前的治疗包括直接将药物注射至眼球内。这














#眼药水#
39
#相关性#
24
#年龄相关#
31
#研发#
30
#年龄相关性黄斑变性#
40
#变性#
26
#黄斑#
23