J Immunother Cancer:基线体重指数(BMI)与晚期非小细胞肺癌(NSCLC)一线免疫联合化疗治疗预后的关系
2022-03-02 yd2015 MedSci原创
研究表明,基线体重指数(BMI)并不影响晚期NSCLC一线接受免疫联合化疗治疗的疗效。
人们已经认识到,在包括非小细胞肺癌(NSCLC)在内的各种恶性肿瘤患者中,体重指数(BMI)增加与免疫检查点抑制剂(ICIs)治疗改善预后相关。然而,目前尚不清楚基线BMI是否会影响晚期NSCLC一线免疫联合化疗治疗的结果。近期,来自意大利团队开展了多中心相关研究,评估基线BMI与晚期NSCLC一线免疫联合化疗治疗时PFS和OS的关系。相关结果发表在Journal for ImmunoTherapy of Cancer杂志上。
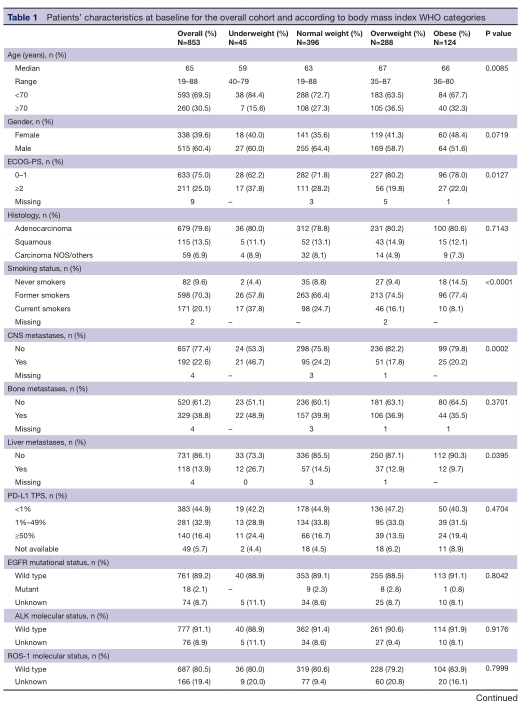
研究纳入853例患者,5.3%患者体重过轻;体重正常者占46.4%;33.8%超重;14.5%患者肥胖。PD- L1表达水平在804例(94.2%)患者中可评估,140例(16.4%)患者PD-L1 TPS≧50%,281例(32.9%)患者为1%-49%,383例(44.9%)患者<1%。超重和肥胖患者更多为年龄≧70岁(p=0.00085),从不吸烟(p<0.0001),更好的EGFR评分(p=0.0127),肝转移比例更低(p=0.0395)。
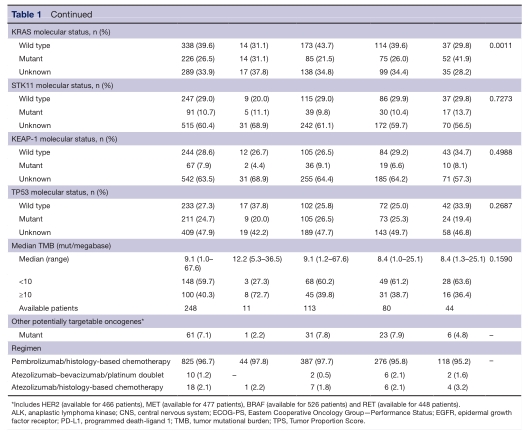
中位随访时间为17.5个月(95% CI 15.9-18.7),整个队列的中位无进展生存期(PFS)和OS分别为7.2个月(95% CI 6.7-7.8)和16.8个月(95% CI 15.2-19.3)。
在体重过轻,正常体重,超重,肥胖患者中位OS分别为15.5个月(95%CI 8.8-15.5),14.6个月(95%CI 13.1-17.2),20.9个月(95%CI 17.3-28.7),和16.8个月(95%CI 12.5-23.2)(log rank:p = 0.045,log rank test for trend:p = 0.131)。中位PFS分别为6.9 个月(95% CI 4.0-14.2),6.6个月(95% CI 5.8-7.3), 8.4个月(95% CI 7.2-9.7),和7.2个月(95% CI 6.0-8.6)(log rank: p=0.123, log rank test for trend: p=0.510)。
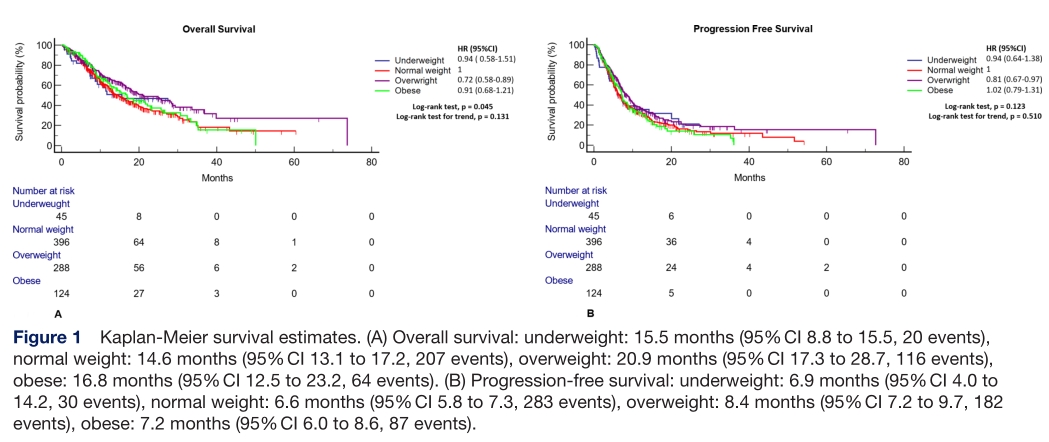
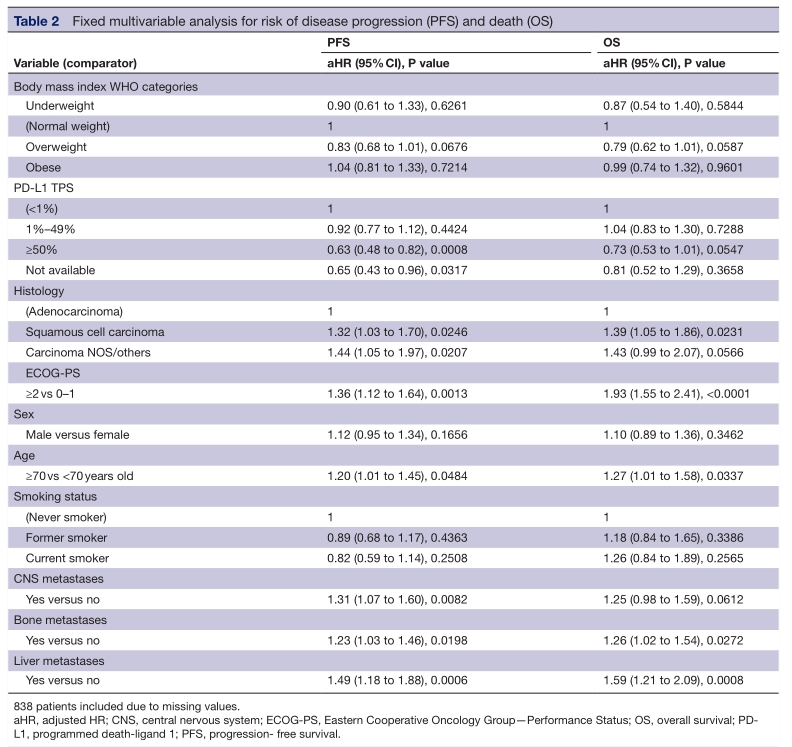
多因素分析发现,基线BMI和临床结果之间没有显著相关。PD- L1表达水平、ECOG- PS、原发肿瘤组织学、年龄、CNS、骨和肝转移被证实是PFS的重要决定因素,而ECOG- PS、原发肿瘤组织学、年龄、骨和肝转移被证实是OS的重要决定因素。
综上,研究表明,基线体重指数(BMI)并不影响晚期NSCLC一线接受免疫联合化疗治疗的疗效。
原始出处:
Cortellini A, Ricciuti B, Vaz VR, et al. Prognostic effect of body mass index in patients with advanced NSCLC treated with chemoimmunotherapy combinations. Journal for ImmunoTherapy of Cancer 2022;10:e004374. doi:10.1136/jitc-2021-004374.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#非小细胞#
28
学习了,谢谢分享
60
学习学习
53
学习了
56
学习
55
学习学习
51
学习
34
学习学习
35
#联合化疗#
40