J Clin Med:新冠患者有长期后遗症发生率状况的系统综述
2022-04-08 网络 网络
随着全球 COVID-19 大流行的发展,很明显,一部分患者在疾病急性期后持续数周或数月出现多器官症状和并发症。对 15 项研究和总共 47,910 名患者进行的系统回顾和荟萃分析测量了超过 50 种
随着全球 COVID-19 大流行的发展,很明显,一部分患者在疾病急性期后持续数周或数月出现多器官症状和并发症。对 15 项研究和总共 47,910 名患者进行的系统回顾和荟萃分析测量了超过 50 种持续性和新患者报告症状的患病率,包括慢性咳嗽、气短、胸闷、认知功能障碍和极度疲劳.在对 57 项研究的另一项系统评价中,包括超过 250,000 名 COVID-19 幸存者,超过一半的人在康复 6 个月后出现了急性后遗症。这种持续的临床表现(通常被称为长期 COVID)的影响和后果越来越引起人们对健康的关注,并对医疗保健系统构成重大挑战。这使得了解导致长期后果发展的因素变得至关重要,这使我们能够识别弱势个体并帮助卫生当局为早期筛查和诊断做好准备,并建立适当的设施来满足他们的需求。对于临床医生而言,识别长期 COVID 风险最大的人群将有助于及时提供适当的干预措施和支持,并以整体患者的视角来降低发病率和改善结果。尽管了解 COVID-19 后遗症的风险因素至关重要,但迄今为止的文献主要集中在持续性体征和症状的普遍性上。一些文献综述提到了预后方面 [4,5,6,7,8,9],但主要作为没有数据综合的叙述性描述,包括异质性研究(考虑不同的人群,例如,有和没有之前的 COVID-19 住院,以及不同的随访时间)。因此,我们进行了这项系统评价和荟萃分析,以确定在因 COVID-19 住院的患者中,哪些因素在住院期间已经存在或出现,与出现新症状或持续症状的风险增加有关。
从两个数据库中共检索到1614篇文章并上传到Rayyan平台。 根据上述标准(995 条记录)的重复和不合格的出版物类型被自动排除。 其余 619 条记录的标题和摘要筛选确定了 117 篇可能符合条件的文章,这些文章接受了全文审查。 共有 97 项研究在适用性评估后被排除(图 1),20 项研究最终被纳入审查和荟萃分析。
研究共纳入 13,340 名患者,其中 6213/13,051(19 项研究中的 47.6%)为女性。 大多数研究发生在欧洲 (11/20, 55%),其次是中国 (8/20, 40%),而一项研究是在南美洲进行的。 20 项研究中有 9 项是多中心的。 大多数是双向的,涉及患者队列或病例系列,其中回顾性收集与急性期(风险因素)相关的数据,并前瞻性记录 PCS 的存在(结果)。 20 项研究中有 8 项采用纵向设计,有一个或多个随访时间点。 通过门诊就诊进行了十项研究,并通过电话采访进行了九项研究; 只有一项研究同时使用了这两种模式。
20 项研究中有 8 项研究了与性别的关联,包括 9421/13,340 (70.6%) 名患者, 47.7% 女性 (4494/9421)。 女性 (2531/4494) 和男性 (2241/4927) 的任何症状发生率为 56.3%。 所有研究均报告女性的 OR > 1(范围 1.15–2.00),总体 OR 具有统计学意义(OR 1.52;95% CI 1.27–1.82)。
1、呼吸系统症状
20 项研究中有 12 项研究了至少一项呼吸系统结局与性别的关联,包括 10,874 /13,340 (81.5%) 名患者。两项研究调查了任何呼吸道症状,而其余研究分析了特定症状,例如呼吸困难、咳嗽和呼吸急促。五项研究发现了具有统计学意义的关联,其中一项与男性相关,四项与女性相关。考虑到个体症状,一氧化碳弥散肺活量 (DLCO) 小于 80% 和喉咙痛表现出接近统计学意义的大 OR (OR 2.28, 95% CI 0.99–5.27 和 OR 1.40, 95% CI 0.94–2.07,分别)。总体分析虽然具有显着的统计异质性(I2 65%,p < 0.01),但证实了呼吸道症状与女性之间关联的显着性趋势(OR 1.20,95% CI 1.00-1.45)。亚组分析证实,除喉咙痛外,所有个体症状的异质性都很高(I2 30-87%)。 图 4 显示了 2530/13340 (19%) 名患者的 20 项研究中的 9 项 (45%) [27,28,34,35,36,39,42,44,46] 探索的与急性疾病严重程度的关联。两项研究 [36,39] 检查咳嗽,五项 [27,28,35,42,46] 检查 DLCO,其余 [34,44] 检查其他呼吸道症状。在亚组分析中,咳嗽和 DLCO 与急性疾病严重程度(严重或危重)具有统计学显着相关性(OR 1.78,95% CI 1.05-3.03;OR 2.05,95% CI 1.06-3.96)。汇总估计值也具有统计学意义(OR 1.66, 95% CI 1.08-2.57),尽管它表现出高异质性(I2 71%)。


2、心理健康症状
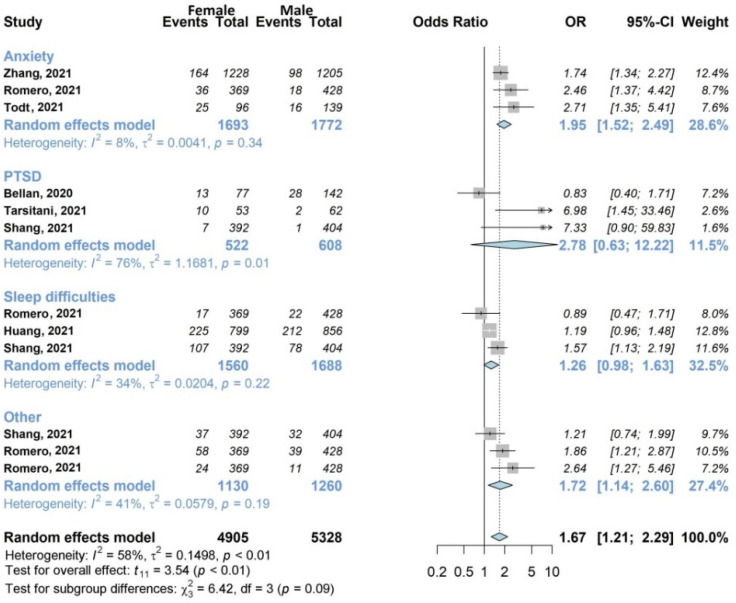
评价中包含 6383/13,340 (47.9%) 名患者 [27,33,38,39,40,41,45] 的七项研究 (35%) 检查了性对心理健康的影响,如图所示 5. 总体分析显示女性的不利影响(OR 1.67, 95% CI 1.21-2.29)。 亚组分析强调了个体症状焦虑的权重,三项研究 [38,41,45] 包括总共 1693/3465 名女性 (48.9%) 进行了调查,并且在统计学上受到女性的影响 (OR 1.95, 95 % CI 1.52–2.49),研究之间的异质性低(I2 8%)。
3、疲劳
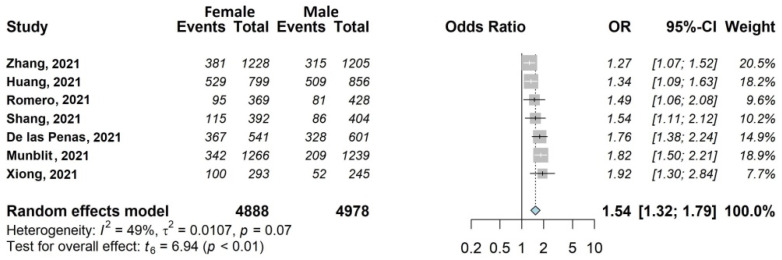
我们发现了七项大型研究 (35%) [30,33,37,38,39,44,45],包括 10,088/13,340 (75.6%) 名符合条件的患者,这些患者检查了女性性别的影响(4895/8724 名女性包括在 分析,56.1%)。 这种关联具有统计学意义,OR 1.54,95% CI 1.32–1.79(图 6)。 如图 7 所示,尽管 OR 为 1.23(95% CI 0.73–2.07),但急性疾病严重程度对疲劳没有显着影响。 二十项 (25%) 研究中的四项 (39,44,45,46] 对这种关联进行了调查,包括 3861/13,340 名患者 (28.9%)。
6月24日,英国卫生部官网发布的最新研究显示,5.8%的新冠患者有长期后遗症,发生长期症状的女性高于男性,而亚裔长期症状的发生率较低。
这项系统评价和荟萃分析表明,女性和急性疾病的严重程度可能使患者易患 COVID-19 的长期症状。 关于该主题的研究存在多个方法学问题,研究之间在考虑的风险因素、定义、随访时间和方式等方面存在很大差异。应鼓励该领域的严谨研究,以具体的科学建议为指导, 帮助医疗保健系统应对感染后可能需要长期护理的越来越多的人的需求。
原始出处:
Maglietta G, Diodati F, Puntoni M, Lazzarelli S, Marcomini B, Patrizi L, Caminiti C.Prognostic Factors for Post-COVID-19 Syndrome: A Systematic Review and Meta-Analysis.J Clin Med. 2022 Mar 11;11(6):1541. doi: 10.3390/jcm11061541
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#发生率#
45
#新冠患者#
70
#系统综述#
47
#后遗症#
48
#Med#
56