J Exp Med:胃癌发生过程中抗病毒通路 与Hippo-YAP通路互作的分子机制
2018-01-30 佚名 上海生科院
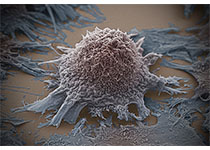
1月16日,中国科学院分子细胞科学卓越创新中心/生物化学与细胞生物学研究所周兆才研究组的最新研究成果,以Targeting IRF3 as a YAP Agonist Therapy against Gastric Cancer为题,在线发表在The Journal of Experimental Medicine上。该项研究揭示抗病毒信号通路对Hippo信号通路的调控作用,特别是IRF3增强YA
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Hippo-Yap#
29
#YAP#
29
学习一下谢谢分享
0
#抗病毒#
26
#互作#
36
#Med#
20
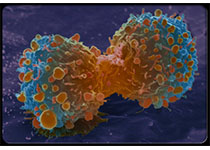
细胞和小鼠胃癌模型表明.敲除IRF3或利用小分子化合物抑制IRF3活性.能够阻滞YAP驱动的胃癌生长.
54