Crit Care:高流量鼻插管与常规氧疗治疗急性加重COPD患者轻度高碳酸血症的疗效比较
2022-04-18 MedSci原创 MedSci原创
在这项多中心随机对照研究中,与COT相比,HFNC并没有减少伴有轻度高碳酸血症的急性加重COPD患者插管的需求。未来的研究应集中于急性加重COPD合并呼吸性酸中毒(pH<7.35)的患者。
无创正压通气(Non-invasive positive pressure ventilation, NPPV)可显著降低急性慢性阻塞性肺疾病(COPD)加重合并呼吸性酸中毒患者的插管需求和住院死亡率。然而,目前不推荐用于轻度高碳酸血症急性COPD加重而无急性呼吸性酸中毒(pH≤7.35)。因此,常规氧疗(COT)是这些患者最常用的标准治疗方法。高流量鼻导管(HFNC)可改善COPD急性加重患者的呼吸功能。然而,其对临床结局的影响尚未确定。
近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,该随机对照试验于2017年7月至2020年12月期间在中国16家三级医院进行的。COPD急性加重并伴有轻度高碳酸血症(pH≥7.35,动脉二氧化碳分压> 45mmHg)的患者随机分为HFNC组和COT组。该研究的主要结局是住院期间符合插管标准的患者比例,次要结局包括治疗失败(不耐受和需要无创或有创通气)、住院时间、住院费用、死亡率和第90天再次入院。
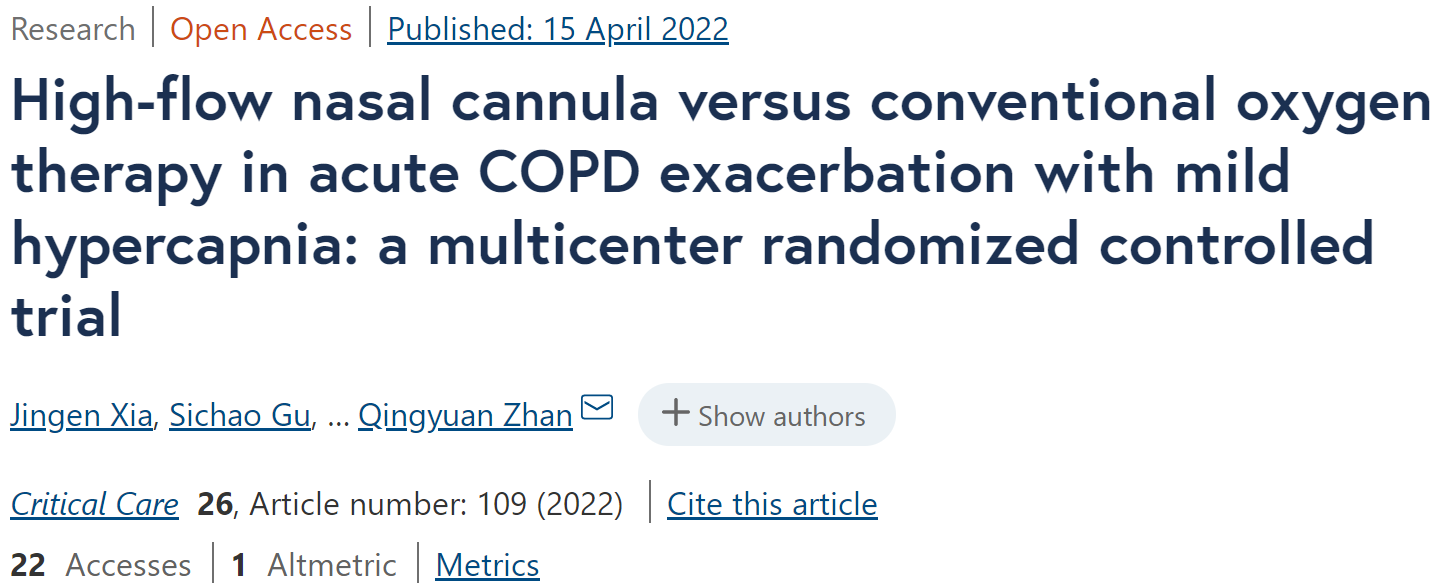
337名随机患者(中位年龄为70.0岁;280人(83.1%);平均pH值为7.399;动脉二氧化碳分压为51 mmHg), 330人完成了试验。4/158例HFNC患者和1/172例COT患者符合插管标准(P=0.198)。
两组进展至NPPV的患者具有可比性(HFNC组15例[9.5%],COT组22例[12.8%];P=0.343)。与COT相比,HFNC组的中位住院时间显著延长(9.0[四分位数范围为7.0-13.0]和8.0[四分位数范围为7.0-11.0]天),中位住院费用较高(约2298美元[四分位数范围为1613-3782美元]和2005美元[四分位数范围为1439-2968美元])。其他次要结局在组间无显著差异。
由此可见,在这项多中心随机对照研究中,与COT相比,HFNC并没有减少伴有轻度高碳酸血症的急性加重COPD患者插管的需求。未来的研究应集中于急性加重COPD合并呼吸性酸中毒(pH<7.35)的患者。然而,由于主要结局率远低于预期,该研究不足以揭示两治疗组之间有意义的差异。
原始出处:
Jingen Xia.et al.High-flow nasal cannula versus conventional oxygen therapy in acute COPD exacerbation with mild hypercapnia: a multicenter randomized controlled trial.Critical Care.2022.https://ccforum.biomedcentral.com/articles/10.1186/s13054-022-03973-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#急性加重#
32
#氧疗#
37
#COPD患者#
42
#高碳酸血症#
35