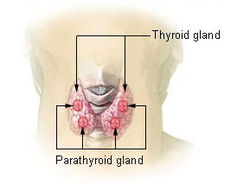
JCEM:甲状腺癌患者放射性碘相关的克隆性造血常见且与存活率降低相关
2018-08-18 xing.T MedSci原创
由此可见,RAI与CH的高患病率相关,CH是血液系统恶性肿瘤的前兆状态。这项研究的意义可能有助于识别接受RAI治疗风险可能超过受益的甲状腺癌的患者的CH。
放射性碘(RAI)在流行病学上与恶性血液病的发生发展有关。克隆性造血(CH)是一种前体克隆状态,会使白血病风险增加,并且相对于其他实体瘤,甲状腺癌患者的白血病发生率有所增加。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在探讨CH的高患病率是否可能是由于RAI暴露引起的,以及CH是否可能是RAI与白血病之间关联的替代指标。
研究人员评估了279例晚期甲状腺癌患者的CH、CH-潜在驱动因子(CH-PD)和总生存期。
甲状腺癌患者的CH患病率为37%,CH-PD的患病率为5.2%。年龄是CH和CH-PD最强的预测因子。对于年龄每增加1岁,CH和CH-PD的几率分别增加5%和13%。即使在调整年龄、外照射放疗和化疗后,RAI剂量与CH和CH-PD显著相关。对于RAI给药剂量每增加10mCi,CH和CH-PD的几率分别增加2%和4%。先前暴露于RAI的CH-PD患者存活率显著较差,即使按年龄进行分层(HR=3.75,95%CI=1.23-11.5,p=0.02)。
由此可见,RAI与CH的高患病率相关,CH是血液系统恶性肿瘤的前兆状态。这项研究的意义可能有助于识别接受RAI治疗风险可能超过受益的甲状腺癌的患者的CH。
原始出处:
Laura Boucai,et al. Radioactive iodine-related clonal hematopoiesis in thyroid cancer is common and associated with decreased survival.J Clin Endocrinol Metab. 2018. https://doi.org/10.1210/jc.2018-00803
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#克隆#
29
#存活率#
37
#JCEM#
32
#JCE#
36
#放射性碘#
39
#克隆性造血#
34
#造血#
32
学习了,谢谢分享
46