必看:2016年宫颈癌临床指南及重大研究进展
2016-12-22 MedSci MedSci原创
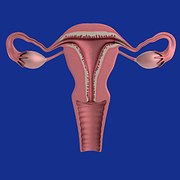
据最新2015中国癌症统计报告显示,在女性特有的肿瘤中,乳腺癌位居第一,宫颈癌第二,是最常见的妇科恶性肿瘤,且发病年龄日益年轻化。2015年国内宫颈癌新发病例估计9.89万例,死亡人数有3.05万例,城市高于农村,考虑到缺乏筛查和治疗的人群,实际发病人数应高于统计数据。下面小编为大家盘点2016宫颈癌临床指南及重大研究进展,供大家学习参考,希望对大家有所帮助。【1】Br J Cancer:宫颈
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#重大研究#
46
#临床指南#
35
学习了
71
谢谢?
68
#研究进展#
36
#宫颈#
27
己阅,谢谢分享
61