Rheumatology:Apremilast单药治疗DMARD无效的活动性银屑病关节炎的长期疗效
2022-03-27 网络 网络
在PALACE 4(第四次PsA长期临床疗效评估研究)中,研究人员对PsA的DMARD无效患者进行了长达5年的Apremilast单药治疗评估,本文报告了评估的结果。
在PALACE 4(第四次PsA长期临床疗效评估研究)中,研究人员对PsA的DMARD无效患者进行了长达5年的Apremilast单药治疗评估,本文报告了评估的结果。
活动性PsA患者随机(1:1:1)接受安慰剂、阿普利司特30毫克或阿普利司特20毫克,每天两次。安慰剂患者在第16周或24周被重新随机分配接受阿普米斯特。双盲阿普利司特持续到第52周,并进行为期4年的开放标签扩展(≤260周的接触)。对第260周的分析是基于观察性数据。
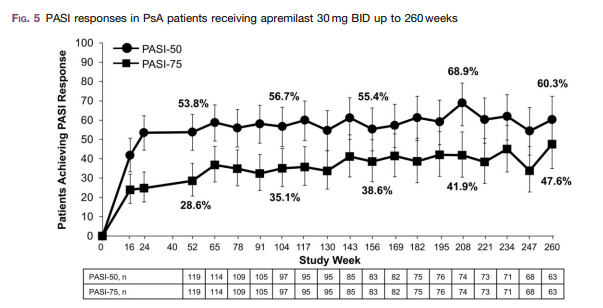
结果,总共有527名患者接受了治疗。在基线时随机选择阿普唑仑30毫克的患者中,45.5%的患者完成了第260周的随访。在研究结束时,24.8%的人报告使用了常规合成DMARD或类固醇。在第260周,分别有65.8%、39.0%和20.3%的阿普利司特30毫克患者分别达到ACR20、ACR50和ACR70的反应。持续治疗后,PsA患者的体征和症状的改善可持续到第260周,包括关节肿胀(84.8%)和压痛(76.4%)次数的减少。在阿普唑仑30毫克患者中,有71.2%的患者的马斯特里赫特强直性脊柱炎关节炎评分为0,95.1%的患者的关节炎计数为0,超过50%的患者达到HAQ残疾指数最小临床重要差异(≥0.35)。在基线银屑病累及体表面积≥3%的患者中,60.3%和47.6%的患者的银屑病面积和严重程度指数得分分别达到≥50%和≥75%的改善。继续服用阿普利司特20毫克的患者也表现出一致且持续的改善。最常见的不良事件是腹泻、恶心、头痛、上呼吸道感染和鼻咽炎。长期来看,并没有发现新的安全问题。
综上所述,该研究结果表明,阿普利司特治疗PsA的疗效可持续到260周,并且耐受性良好。
原始出处:
Alvin F Wells, et al., Apremilast monotherapy for long-term treatment of active psoriatic arthritis in DMARD-naïve patients. Rheumatology (Oxford). 2022 Mar 2;61(3):1035-1043. doi: 10.1093/rheumatology/keab449.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Apremilast#
37
#REM#
40
#单药治疗#
48
#活动性#
48
#Rheumatology#
40
#AST#
21
#关节炎#
36
#活动性银屑病关节炎#
40
#长期疗效#
34
#DMARD#
42