lancet oncol:派姆单抗(pembrolizumab)在局部晚期或转移性尿路上皮癌患者中安全性和活性的1期临床研究(KEYNOTE-012)
2017-01-17 MedSci MedSci原创
PD-1及其配体在尿路上皮癌中表达,研究已经发现抑制PD-1途径具有临床益处。近期一项发表在LANCET ONCOL杂志上的文章研究评估了抗PD-1抗体派姆单抗(pembrolizumab)在局部晚期或转移性尿路上皮癌患者中的安全性和活性。这项研究是非随机,多组群,开放标签,1b期试验研究。研究者们从美国和以色列的8家医院招募了18岁及以上的患者,进行组织学或细胞学证实的局部晚期或转移性尿路上皮癌
PD-1及其配体在尿路上皮癌中表达,研究已经发现抑制PD-1途径具有临床益处。近期一项发表在LANCET ONCOL杂志上的文章研究评估了抗PD-1抗体派姆单抗(pembrolizumab)在局部晚期或转移性尿路上皮癌患者中的安全性和活性。
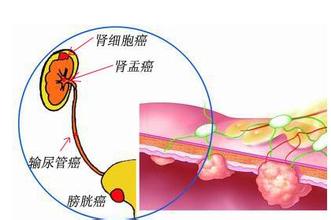
这项研究是非随机,多组群,开放标签,1b期试验研究。研究者们从美国和以色列的8家医院招募了18岁及以上的患者,进行组织学或细胞学证实的局部晚期或转移性尿路上皮癌(包括肾盂,输尿管,膀胱或尿道癌)的诊断。通过免疫组织化学的方法,至少在患者肿瘤细胞或肿瘤基质中检测到1%的PD-L1表达。
每2周静脉内给予患者派姆单抗(10mg / kg),直到疾病进展或不可接受的毒性作用或研究结束(即24个月的治疗)。主要终点是通过掩蔽的,独立的中心综述评估的安全性和总体反应(由实性肿瘤中的反应评价标准[RECIST]版本1.1定义)。
在接受一个或多个剂量的派姆单抗(所有患者治疗群体)的患者中评估安全性;在接受派姆单抗的患者中评估活性,这些患者在基线时具有可测量的疾病,并且具有一个或多个基线后扫描,或由于进行性疾病或治疗相关不良事件(全分析集)而停止的患者。
此项研究结果显示:在2013年5月14日至2013年12月10日期间,115名患者作为两部分同意过程的一部分进行了组织预筛选。 61例(53%)患者为PD-L1阳性,其中33例纳入研究。所有入选患者接受至少一次剂量的派姆单抗,并进行了安全性分析。 27名患者评估了活性。 6名患者无法评估:3名患者由于在第一次基线后扫描之前有非治疗相关的不良事件,2名患者在第一次基线后扫描前退出,以及1名患者在基线时没有可测量的疾病。
最常见的治疗相关不良事件是疲劳(33名患者中的6名[18%])和外周水肿(4名[12%])。 5名(15%)患者有11个3级治疗相关不良事件;在1名以上的患者中没有发生单一事件。三名(9%)患者经历了5个严重的治疗相关不良事件。在中位随访13个月(范围1-26,IQR 5-23)后,27例可评估患者中有7例全部反应(26%[95%CI 11-46]),其中3例完全反应(11% [2-29]),4例(15%[4-34])部分反应。在研究期间4名患者死亡(心脏骤停,肺炎,败血症和蛛网膜下腔出血)中,没有一个被认为是治疗相关的。
此项研究结果表明:派姆单抗(Pembrolizumab)在晚期尿路上皮癌患者中显示出抗肿瘤活性和可接受的安全性,需要对此人群中派姆单抗进行2期和3期的研究。
原始出处:
Plimack ER, Bellmunt J, Gupta S, Berger R, Chow LQ, Juco J, Lunceford J, Saraf S, Perini RF, O'Donnell PH.Safety and activity of pembrolizumab in patients with locally advanced or metastatic urothelial cancer (KEYNOTE-012): a non-randomised, open-label, phase 1b study. Lancet Oncol. 2017 Jan 9. pii: S1470-2045(17)30007-4. doi: 10.1016/S1470-2045(17)30007-4.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
28
#PE#
34
#Pembro#
38
#mAb#
26
#KEYNOTE#
37
#Oncol#
19
#局部晚期#
29
谢谢啦谢谢分享
81
#局部晚期或转移性尿路上皮癌#
30
临床试验
76