Nat Commun: 使用微流体蛋白质印迹分析循环肿瘤细胞中的蛋白质表达
2017-03-27 MedSci MedSci原创
循环肿瘤细胞(circulating tumor cells,CTCs)是指从原生肿瘤或转移性肿瘤脱离并进入血液循环系统的肿瘤细胞。透过观察循环肿瘤细胞的数量变化以及分析它们的基因特性,可以帮助判断病情以及决定治疗方针。 液循環系統轉移並在其中存活、移出血管、最後在新的部位停下來增生成新的腫瘤。 進入到血液循環系統的腫瘤細胞被稱為循環腫瘤細胞 (circulating tumor cells,
循环肿瘤细胞(circulating tumor cells,CTCs)是指从原生肿瘤或转移性肿瘤脱离并进入血液循环系统的肿瘤细胞。透过观察循环肿瘤细胞的数量变化以及分析它们的基因特性,可以帮助判断病情以及决定治疗方针。
恶性肿瘤都会通过血液传播转移到身体的其他器官,而肿瘤转移是导致肿瘤患者死亡的主要原因。肿瘤细胞侵入到原发肿瘤细胞的周围组织中,进入血液和淋巴管系统,形成循环肿瘤细胞CTC,并转运到远端组织,再渗出,适应新的微环境,最终"播种"、"增殖"、"定植"、形成转移灶。因此早期发现血液中的CTC,对于患者预后判断、疗效评价和个体化治疗都有着重要的指导作用。
CTC是从肿瘤流入循环的稀有细胞,在每7.5ml血液中仅有1-500个细胞。因此,大量研究集中在通过利用这些癌细胞的独特特征(例如表面蛋白表达,大小和变形性)来分离CTC, CTC高计量值与低生存率和对治疗的低应答率相关。此外,通过新一代测序表徵CTC,确定了CTC与其原发性肿瘤之间的基因表达不一致。这些研究表明, CTC可能存在不同的亚群并有助于肿瘤的转移。然而,虽然CTC计数和基因组学可以区分鉴别部分亚群,但不能描述所有表型。事实上,最近的研究表明,在某些情况下,基因组学/转录组学和蛋白质表达之间的相关性很弱。
然而,与单细胞基因组学和转录组学不同,单细胞蛋白测定的进展滞后。令人瞩目的是,大多数单细胞蛋白测定(对于未修饰的内源性靶标)是单级免疫测定,包括酶联免疫吸附测定和免疫细胞化学,以及一种可以进行高通量的单细胞蛋白质组空间分析的质谱流式细胞仪。CTC蛋白质分析主要集中在表面和分泌蛋白上。但重要的是,复合和测定各种蛋白质靶标(包括细胞内信号通路)的能力受到限制。在单个CTC中直接测量多种蛋白是单个CTC转录组学、基因组及计数研究的关键。
然而,通过单级免疫测定的靶标检测仍受到免疫反应物的特异性和可用性的限制。这些局限性在两个关键方面阻碍了对CTC表型的了解。首先,单阶段免疫测定对于每个单细胞的表面和细胞内蛋白质的多重测量是困难的。实体瘤和CTC通过免疫测定分类(即CK +,EpCAM +和CD45-表达)。但临床免疫测定(例如,免疫组织化学)由于常规过滤器组的光谱成像限制而限于5种蛋白质并且难以"去染色"细胞(去除抗体探针)。流式细胞仪也有多种缺点,特别是细胞内蛋白质靶标。更重要的是,由于细胞处理损失和死体积,流式细胞术和质粒细胞计都不能检测少数CTC。其次,如果高特异性探针不可用,免疫测定不能唯一地检测蛋白质。这在癌症中尤其重要,因为异构体的表达越来越多地影响患者的预后,而关键异构体没有可用的特异性抗体。质谱仪虽能检测出大部分的蛋白异构体,但是对关键信号蛋白的分析灵敏度有限。
数年来,研究人员利用Western Blot进行蛋白质的分离。在免疫测定之前通过分子量(或迁移率)使蛋白质分离从而可以监定脱靶的和与抗体非特异性结合的蛋白。通过大小空间分辨蛋白质首先允许单个抗体探针检测多种不同的蛋白质形式。然而,这种蛋白印迹分析的灵敏度低,需要合并细胞使蛋白质达到一定含量才可检测到,这掩盖了重要的CTC至CTC蛋白表达水平的变化。为了克服这个差距,我们最近推出了针对数千个单个培养的神经乾细胞和胶质母细胞瘤细胞中的每一个蛋白质表达进行优化的单细胞分辨率蛋白质印迹。然而,单细胞蛋白质印迹的当前格式需要1000s细胞来解决沉降到微孔中时的细胞损失。
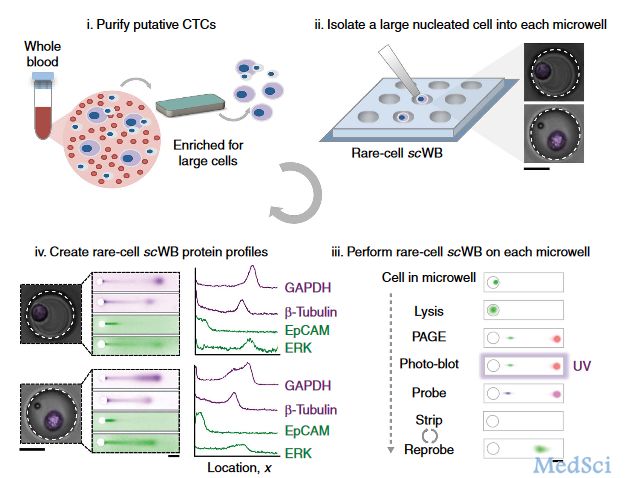
在这里,我们介绍一种稀有细胞,单细胞分辨率蛋白质印迹(scWB)来测量从原发性雌激素受体阳性(ER +)乳腺癌患者体内分离的单个CTC中的一组蛋白质。稀有细胞scWB可以量化多个表面和细胞内信号蛋白--与我们设定的仪器定量限相比,每个单独的CTC中允许出现CTC之间的生物蛋白表达差异。我们发现罕见细胞scWB与建立的CTC隔离工具兼容,因此成功地用少至两个起始细胞分析CTC群体。在对ER +转移性乳腺癌患者衍生的CTC进行的初步研究中,我们观察到难裂解的CTC表型,以及通过每次测定分析的CTC数量来归一化靶蛋白表达的独特能力,这里只有一个CTC。罕见细胞scWB提供了一种新的方法来检查四氯化碳,具有相关性,从了解CTC生物学到监测个体对治疗的反应。
稀有细胞scWB量化多个表面和细胞内信号蛋白 - 在每个单独的CTC中,允许估计CTC之间的生物蛋白表达变化,与我们建立的技术变异的定量阈值相比。我们显示罕见细胞scWB与建立的CTC隔离工具兼容,因此成功地用少至两个起始细胞分析CTC群体。在对ER +转移性乳腺癌患者衍生的CTC进行的初步研究中,每个微孔板中含一个细胞,结果我们观察到CTC表型难裂解,且这一特性可以使每次实验中的多个CTC中的靶蛋白均能正常表达。因此,稀有细胞scwb为CTCs的检测提供了一种新的方法,利用CTC的生物学信息监测个体对治疗的反应。
原文出处:Elly Sinkala et al. Profiling protein expression in circulating tumour cells using microfluidic western blotting, Nature Communications (2017)
此文系梅斯医学(MedSci)原创编译整理,转载需授权!
Read more at: https://medicalxpress.com/news/2017-03-sample-blood-probe-cancer-clues.html#jCp
Read more at: https://medicalxpress.com/news/2017-03-sample-blood-probe-cancer-clues.html#jCp
Read more at: https://medicalxpress.com/news/2017-03-sample-blood-probe-cancer-clues.html#jCp
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
29
#COMMUN#
28
#白质#
37
#蛋白质#
28
#肿瘤细胞#
32
#循环肿瘤细胞#
0