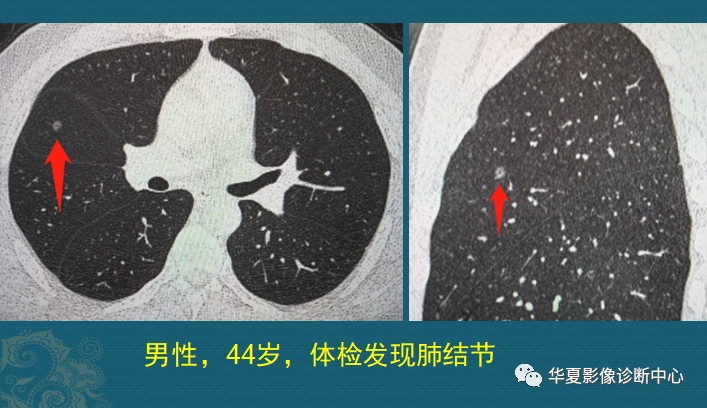
44岁男子,体检发现肺结节。该男子不吸烟,没有咳嗽、咳痰等肺部症状,单位组织体检,发现右肺一个小结节,直径接近5mm:
小于5mm的肺结节都是低危结节,首选随访观察,一般低危结节每年复查一次就好。但这个结节有2个地方要重视:
(1)中央有关小空泡征,仔细看箭头指的位置,里面有个小黑点。
空泡征不止见于早期肺癌,良性病灶也可以见到,但概率不同:炎性结节出现率约5%,早期普通型腺癌约50-60%,而早期粘液腺癌结节估计在10%左右。
(2)结节内有血管进入,看右图矢状位切面,下缘有一根很细的小血管进入结节。
结节进入也不止见于早期肺癌,但如果进入后变得增粗、边缘模糊,要警惕恶性的可能。
鉴于这2个特征,因此推荐他3-6个月复查(如果是老烟民,通常推荐3个月复查,烟草毒雾会让某些肺结节加速)。6个月后,他回来复查了CT:
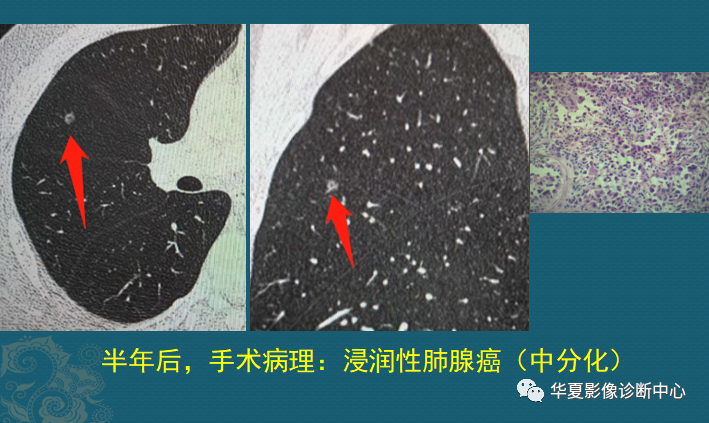
目测结节稍微有一点点增大,但测量直径仍为5mm,不能排除测量误差。他权衡了一下,选择胸腔镜手术切除,病理是浸润性肺腺癌,腺泡型(相当于中分化),清扫肺门及纵隔淋巴结未见转移。这种类型的远期治疗效果也非常好!
5mm的肺结节,病理结果是浸润性肺腺癌,这种情况还是非常少见的。
1、从1个癌细胞,长成晚期肺癌,大概需要多久?
肺癌的发展速度是不一致的,有些幸运的“懒癌”患者,可以几年甚至十几年无明显进展,这种的不可怕;而有的肿瘤从很小时候就具备快速增长的能力,需要重点监控!
我们搜索了最近3年的肺结节病例,找到两个速度最快的肺癌病例,我们来看看它俩的生长速度,了解查体的意义以及最适宜的查体频率。
病例1:肺腺癌,3.5年
这是一位70多岁老人,前列腺手术后定期体检,2016年基本正常,2017年右下肺出现4mm肺结节,2018年结节增大到5mm,之后隔了1年零9个月再次复查,结节增大到1.5cm,并出现分叶、毛刺等恶性征象,没有发生肺门、纵隔淋巴结转移,也没有远处转移。

这是一个肺腺癌结节,从1个癌细胞长到1.5cm,用了大概3.5年;早期比较慢,长到5mm用了20个月,从5mm长到1.5cm,用了21个月。注意:这几乎是最快的速度了!绝大部分肺结节的增长速度,要慢于这个速度!
病例2:肺鳞癌,3年零10个月
68岁老人,老烟民,因为冠心病住院,首次胸部CT看不到明显异常,之后逐渐出现肺结节:
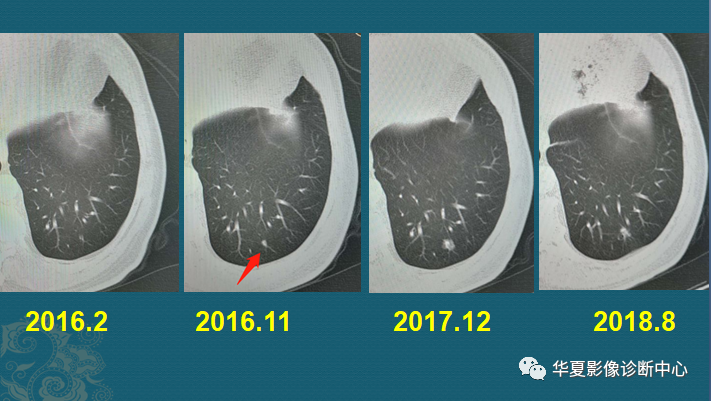
在9个月时间里长出3mm肺结节,又隔了13个月,增大到8mm,之后再过了8个月,结节却萎缩变小了一点(大约7mm)。随访过程中逐渐增大的肺结节,要提升危险等级,积极处置。
有的肺结节暂时性缩小并不提示良性,之后过了1年零2个月,它猛然增大成一个不规则肿块,直径3cm,表面有分叶,并且牵拉胸膜了(下图)。
一年多的时间快速增大,提示肿瘤已经进入加速期,这时候如果继续放任不管,肿瘤会展露凶残的真面目的!只过了2个月,肿瘤再次以肉眼可见的速度增大,并且发生了胸膜结节状转移(右图蓝箭头),病理穿刺是低分化肺鳞癌。

在工作中发现,很多老烟民的肺结节,生长速度更快一些,似乎烟草毒素能为癌细胞提速。所以长期吸烟的人首次发现肺小结节,通常应建议患者复查间隔稍短一点,避免漏掉这种快速型结节。当然这种类型的很少!
以上两个结节,病理分别是肺腺癌和肺鳞癌,都是在3年多的时间里从无到有,到浸润期。
2、肺结节的平均生长速度是多少?
肺结节平均生长速度这方面的数据,国内外都有不少,甚至对于肺结节的细节研究,国内很多医院做得很好,很多细节是领先国外的。
肺结节的体积倍增时间(VDT):指肿瘤体积增长一倍所耗费的时间(以月或天为单位计算),代表肿瘤细胞的活跃程度和侵袭力。
实际上对肺结节增长的判定有很多种方法,不同研究团队的数据有一定差异。大家可以化繁为简,参考下面这个数据:
-
实性肺结节,平均倍增时间为149天;
-
纯磨玻璃结节,平均倍增时间为813天;
-
混合性磨玻璃结节,平均倍增时间为457天。
对于实性肺结节,随访2年以上未见增大,良性可能大;对于磨玻璃结节,因为倍增时间长,随访时间要大于2年,甚至建议长期随访。
其中磨玻璃结节中,结节的直径、混合磨玻璃结节中实性成分的大小、吸烟和既往有肺癌史,是结节生长的危险因素。
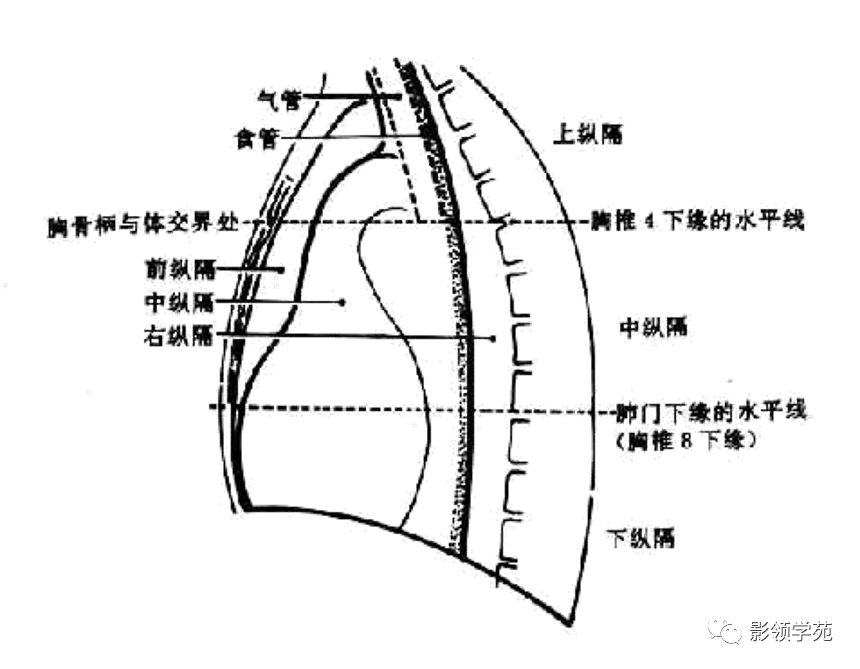
3、检查发现肺结节怎么处理?
(1)长径≤10 mm的实性肺结节管理

(2)长径>10 mm的实性肺结节管理与诊治
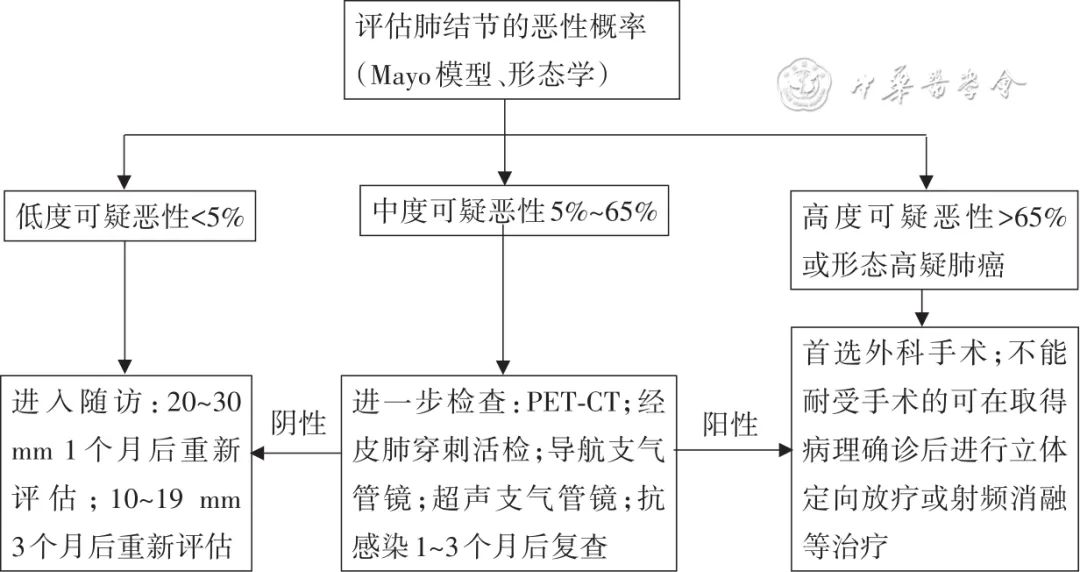
(3)亚实性肺结节管理与诊治(磨玻璃结节,包括pGGN和mGGN),pGGN为纯磨玻璃结节,又称非实性结节;mGGN为混杂磨玻璃结节,又称部分实性结节;

(4)新发肺结节管理与诊治
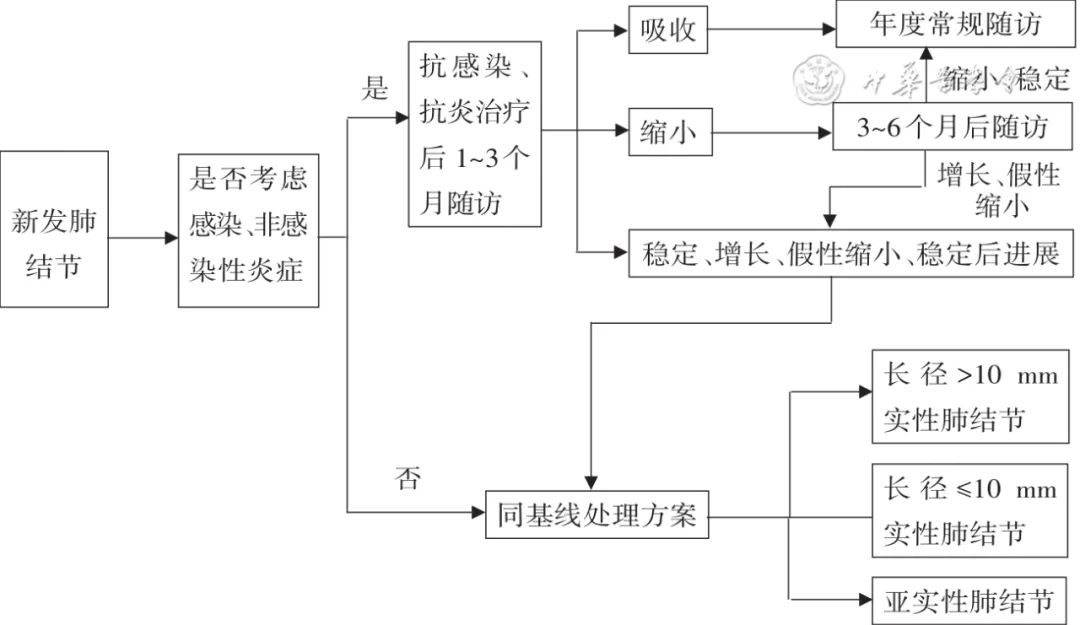
(5)多发性肺结节管理与诊治原则
-
多发性肺结节建议单独评估每个结节,并筛选出优势结节(优势结节为最可疑的结节,其不一定是最大的结节);多发性肺结节的处理,原则上应根据优势结节的情况采取相应临床策略。
-
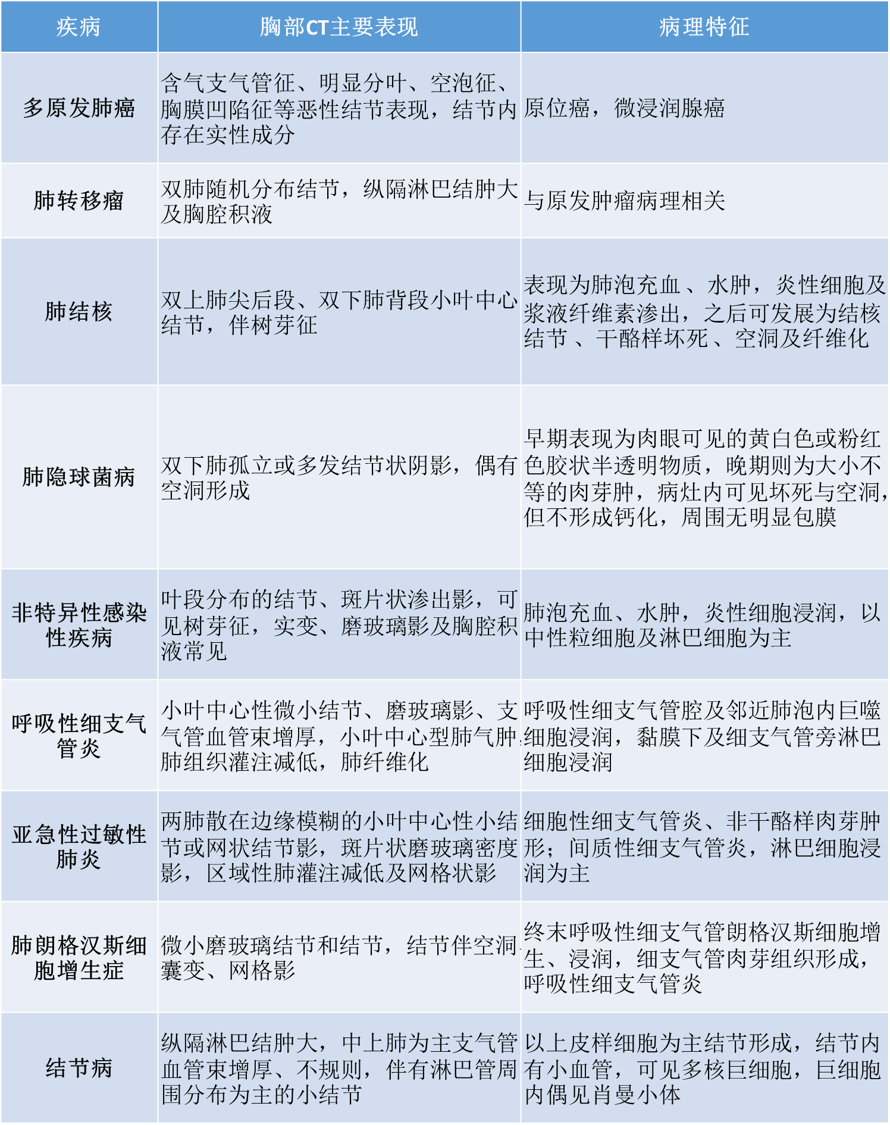
对于多发性实性肺结节,应考虑肺转移瘤、感染性肉芽肿(如结核、真菌)、非感染性肉芽肿等。PET-CT有助于判断转移性结节及其原发灶,对多发性肺结节诊疗有一定价值;且在绝大多数情况下,转移灶3个月内可以明显观察到增大。
-
对于多发性亚实性肺结节,应考虑多原发肺癌、感染性炎症、非感染性炎症等。如病灶在3个月首次随访CT后无明显减小、变淡或吸收,应考虑多原发肺癌的可能性;但PET-CT对于多发性亚实性肺结节的判断有局限性。
-
对于多发性肺结节进行分类和采取最佳治疗存在困难时,建议MDT。
多发性肺结节影像表现及病理特征
参考文献
中国县域医院肺癌筛查共识编写专家组, 中华医学会呼吸分会肺癌学组. 中国县域肺癌筛查共识(2020年)[J] . 中华医学杂志, 2021, 101(14) : 979-988. DOI: 10.3760/cma.j.cn112137-20201130-03227.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#小结节#
48
学习
41
#肺结节#发展成#肺癌#
104
好文。
43
学习了
50