BMC Cancer:中肿团队HER2阳性难治性转移性乳腺癌转化模式疗法疗效显著
2022-03-16 yd2015 网络
研究表明,HER2阳性难治性转移性乳腺癌进展后使用拉帕替尼联合卡培他滨或长春瑞滨疗效显著。
尽管人表皮生长因子受体2 (HER2)阳性乳腺癌HER2阻断能显著提高生存期,但对抗HER2治疗的耐药性仍然不可避免。TDM-1是标准的二线治疗。当其他抗HER2治疗不可用时,患者进展后可以继续使用曲妥珠单抗抗her2治疗,但疗效有限。因此,来自中山大学肿瘤防治中心的团队开展了一项II期临床研究(sysucce -005),旨在探索切换模式对HER2阳性难治性转移性乳腺癌的有效性。相关结果发表在BMC Cancer杂志上。
研究纳入中国6家医院曲妥珠单抗治疗快速进展的HER2阳性转移性乳腺癌患者,转向口服拉帕替尼1250mg qd +卡培他滨(每天1000 mg / m2 bid d1-d14)或长春瑞滨(25 mg / m2/次,静脉注射,d1和d8,每21天为一周期)。主要终点为无进展生存期(PFS)。
2015年1月5日至2020年5月31日,纳入159例患者。平均年龄47.3岁(24 -75岁)。47.2%的患者(75/159)为绝经前,66.0%的患者(105/159)为激素受体(HR)阴性。超过一半的患者(63.5%)发生内脏转移,23.3%的患者发生脑转移。卡培他滨和长春瑞滨治疗分别有67.9%(108/159)和32.1%(51/159)的患者。
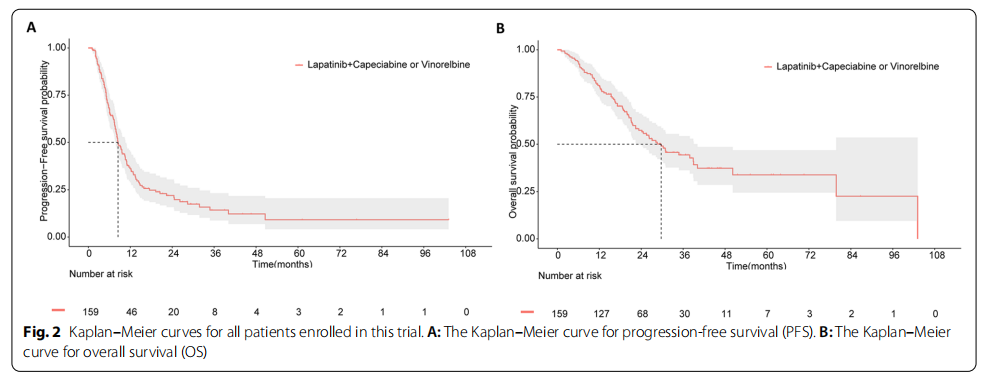
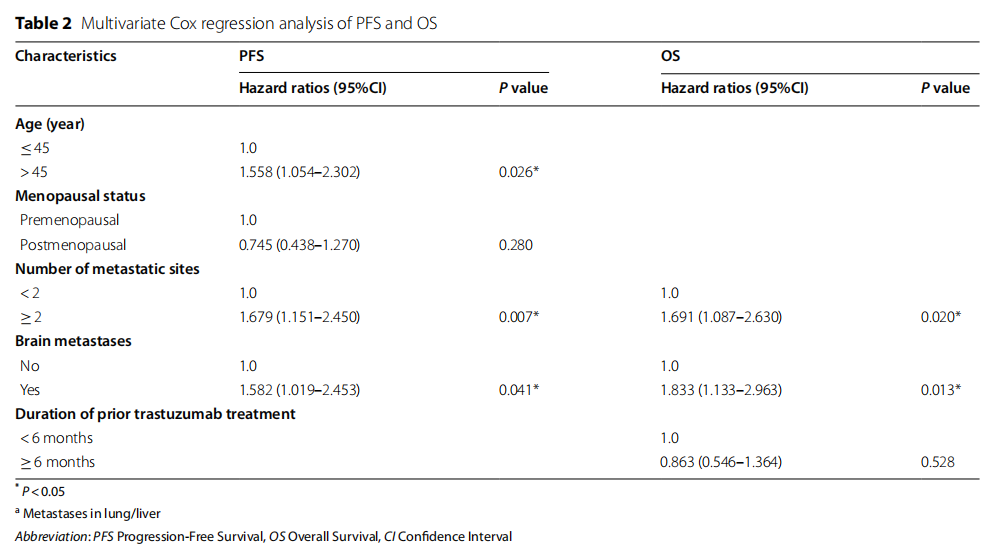
中位随访为33.1个月,中位PFS和OS分别为8.5个月(95% CI 7.2-9.8)和29.7个月(95% CI 21.9-37.5)。此外,多因素Cox回归分析,发现脑转移(PFS: HRs=1.582, 95% CI 1.019-2.453, P=0.041;OS: HRs=1.833, 95% CI 1.133 -2.630, P=0.013)和≧2个转移灶(PFS: HRs=1.679, 95% CI 1.151- 2.450, P=0.007;OS: HRs=1.691, 95% CI 1.087 -2.630, P=0.020)是独立预后因素。
在159例可评估患者中,RR为29.6% (95% CI 22.6-37.3)。无患者获得CR。PR、SD和PD分别为47(29.6%)、51(32.1%)和24(15.1%)例。CBR为61.7%。
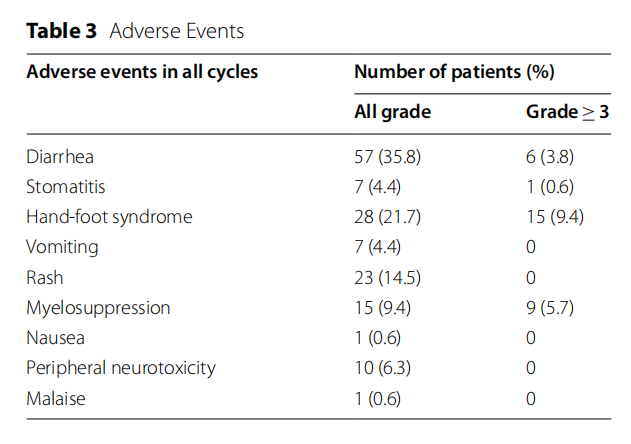
最常见的AEs为腹泻和手足综合征,但3级及以上的AEs分别仅占3.8%和9.4%。11.3%(18/159)因AEs停止拉帕替尼。未观察到治疗相关的死亡或危及生命的AEs。
综上,研究表明,HER2阳性难治性转移性乳腺癌进展后使用拉帕替尼联合卡培他滨或长春瑞滨疗效显著。
原始出处:
Fangfang Duan, Muyi Zhong, Yuyu Ma, et al. The efcacy of human epidermal growth factor receptor 2 (HER2) blockade switching mode in refractory patients with HER2-positive metastatic breast cancer: a phase II, multicenter, single-arm study (SYSUCC-005). BMC Cancer (2022)22:271. https://doi.org/10.1186/s12885-022-09399-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BMC#
47
#HER2阳性#
0
#转移性#
38
#难治性#
46