J Clin Oncol:随机FinXX研究超10年OS结果表明加用卡培他滨至辅助化疗中可改善早期乳腺癌患者的预后
2022-01-14 yd2015 MedSci原创
FinXX研究表明,在辅助化疗的基础上加用卡培他滨可改善早期乳腺癌患者的预后。
FinXX是一项随机、开放标签、多中心试验,主要是评估在含紫杉烷和蒽环类药物的辅助化疗方案基础上加用卡培他滨治疗早期乳腺癌的疗效。近期,Journal of Clinical Oncology杂志上发表了其随访超10年的OS结果。
在2004年1月27日和2007年5月29日之间,1500名腋窝淋巴结阳性或高危淋巴结阴性的早期乳腺癌患者被纳入。患者被随机分配至: TX-CEX组(3周期多西他赛+卡培他滨,接着3周期环磷酰胺+多柔比星+卡培他滨;n=753例)和T-CEF组(3周期多西他赛,接着3周期环磷酰胺+多柔比星+氟尿嘧啶;n=747例)。基于超过15年的随访时间比较两组的OS。
数据收集于2020年12月31日锁定。研究开始时的中位年龄为53岁(TX-CEX组,52岁;T-CEF组,53年;两组中位肿瘤直径均为22 mm (P=0.842)。大多数患者(n=1,142例,76.4%)为ER阳性,282例(18.9%)为HER2阳性。到目前为止,存活患者的中位随访时间,TX-CEX组为15.3年(四分位数范围,14.5-16.1年),T-CEF组为15.4年(四分位数范围,14.8-16.0年)。
在随访期间,375例(25.1%)患者死亡,其中TX-CEX组171例(22.8%),T-CEF组204例(27.4%)。与T-CEF组相比,TX-CEX组的OS显著延长(HR 0.81;95% CI, 0.66 ~ 0.99;log-rank检验P =0.037;Gehan-Breslow- Wilcoxon检验P=0.044)。
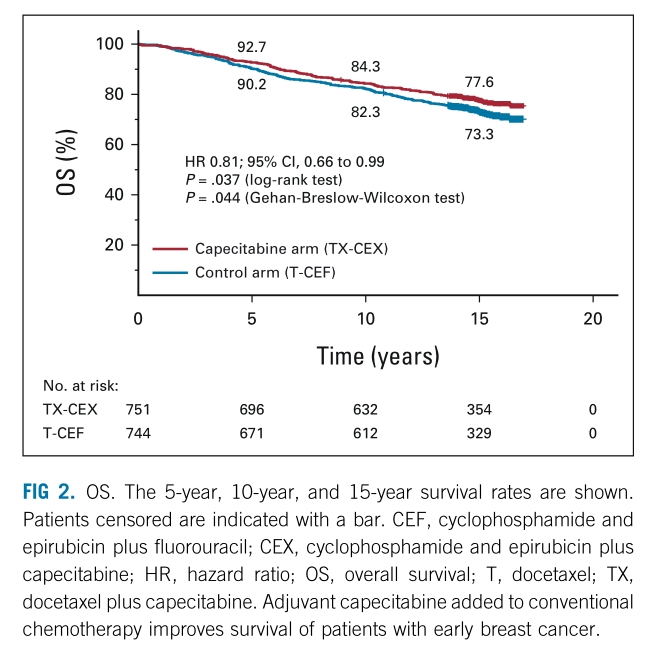
两组OS差异
TX-CEX和T-CEF组的5年、10年和15年OS率分别为92.7%和90.2%,84.3%和82.3%,以及77.6%和73.3%。
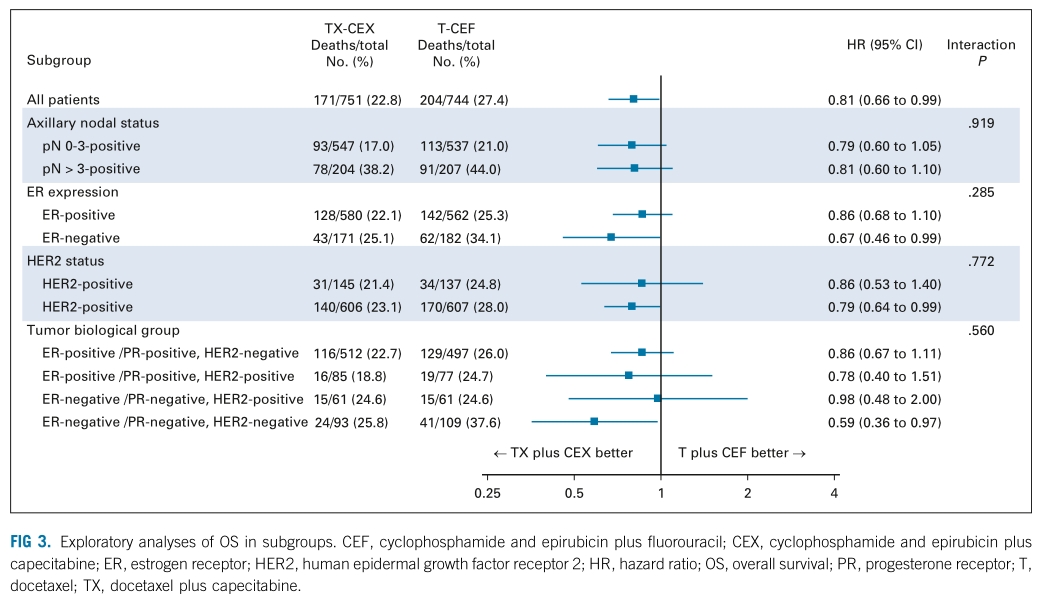
OS亚组分析
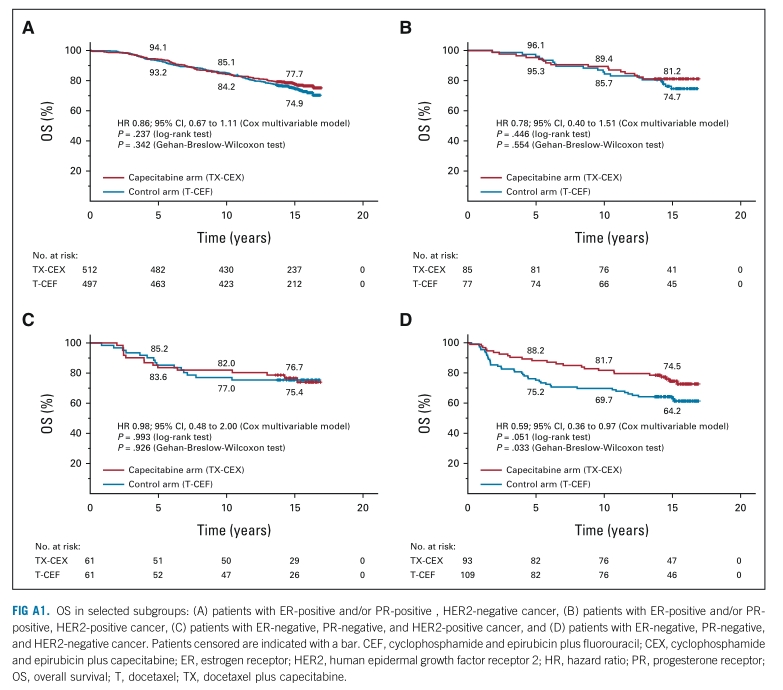
TNBC亚组患者中, TX-CEX组的5年,10年,15年生存率分别为88.2%,81.7%,和74.5%,而T-CEF组的分别为75.2%,69.7%和64.2% (HR 0.59; 95% CI, 0.36 ~ 0.97;log-rank检验P =0.051;Gehan-Breslow-Wilcoxon检验P=0.033)。
OS亚组分析
综上,FinXX研究表明,在辅助化疗的基础上加用卡培他滨可改善早期乳腺癌患者的预后。
原始出处:
Joensuu H, Kellokumpu-Lehtinen PL, Huovinen R, Jukkola A, Tanner M, Ahlgren J, Auvinen P, Lahdenperä O, Villman K, Nyandoto P, Nilsson G, Poikonen-Saksela P, Kataja V, Bono P, Junnila J, Lindman H. Adjuvant Capecitabine for Early Breast Cancer: 15-Year Overall Survival Results From a Randomized Trial. J Clin Oncol. 2022 Jan 12:JCO2102054. doi: 10.1200/JCO.21.02054. Epub ahead of print. PMID: 35020465.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
0
#卡培他滨#
42
#乳腺癌患者#
47
学习了
49