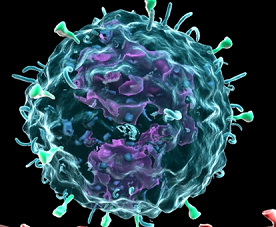
Science:新型CD4 T细胞亚群调节肠道炎症反应
2016-06-06 佚名 生物谷
外周调节性T细胞(pTreg)对于限制由外源物质引起的炎症反应具有重要的作用。在肠道中,pTreg主要存在于固有层(lamina propria)中,而上皮间存在的CD4 T细胞同样具有抑制炎症反应的作用。这部分CD4 T细胞依赖视黄酸(Retinoic Acid)以及转化生长因子(TGF-b)发挥功能。为了研究肠道的炎症稳态调节过程中,pTreg以及CD4细胞分别发挥了怎样的作用,来自洛克

外周调节性T细胞(pTreg)对于限制由外源物质引起的炎症反应具有重要的作用。在肠道中,pTreg主要存在于固有层(lamina propria)中,而上皮间存在的CD4 T细胞同样具有抑制炎症反应的作用。这部分CD4 T细胞依赖视黄酸(Retinoic Acid)以及转化生长因子(TGF-b)发挥功能。为了研究肠道的炎症稳态调节过程中,pTreg以及CD4细胞分别发挥了怎样的作用,来自洛克菲勒大学的Daniel Mucida与Bernardo S. Reis课题组进行了深入研究,相关结果发表在最近的Science杂志上。
首先,作者利用双光子显微镜对小鼠肠道内的Treg细胞进行了动态追踪。结果显示,大部分Treg细胞分布于固有层(68%)以及肠道上皮层(14%)。剩下的18%的Treg细胞虽然一直处于迁移的状态,但它们进入固有层的频率明显高于肠道上皮层。由于体外实验显示Treg在肠道上皮中的含量一直很低,这说明Treg细胞要么发生了凋亡,要么转变成其它类型的细胞。
虽然所有的Treg细胞都表达转录因子ThPOK,但小肠上皮层中的CD4T细胞中ThPOK的表达量却很低。 作者怀疑ThPOK的下调与CD4 T细胞的动态变化之间存在联系。它们利用OT-II小鼠进行试验,通过向这类小鼠进行OVA刺激,能够诱导其体内的T细胞下调ThPOK的表达。作者向全身性表达RFP的OT-II小鼠体内转入ThPOK-GFP融合蛋白,再分选出天然的T细胞(RFP/GFP双阳性)打入Rag 1 ko小鼠体内,经过一周饲喂含有OVA的饲料后,作者追踪了这部分细胞并通过计算机进行了后续分析。结果显示,在经过OVA刺激后,打入的T细胞ThPOK的表达量明显下降。在那些ThPOK表达量仍较高的细胞群体中,仅有20%停留在小肠上皮层中。这说明在这一环境中,部分的T细胞要么下调了ThPOK的表达,要么发生了凋亡。
进一步,作者发现在小肠上皮中有相当一部分的Treg细胞FoxP3的表达量发生了明显的下调,它们转变为一种特殊的CD4 T细胞类型。
之后,作者发现这部分CD4 T细胞的数量在无菌小鼠中发生了明显的减少(约10倍)。通过抗生素处理,作者发现这一处理能够抑制Treg中FoxP3的下调,从而提高小肠上皮层中Treg细胞的数量。而ThPOK对于促进Treg向CD4 细胞的转化具有关键的作用。作者通过条件性敲除小鼠中的Treg细胞中的T-bet,发现这一转化效应出现了明显的降低,这说明Tet有可能通过下调ThPOK起到转变Treg表型的作用。
最终,作者证明了这部分特殊的上皮内的CD4 T细胞与组织适应性Treg细胞通过调节了肠道的炎症反应。
原始出处:
Sujino T, London M, Hoytema van Konijnenburg DP, Rendon T, Buch T, Silva HM, Lafaille JJ, Reis BS, Mucida D. Tissue adaptation of regulatory and intraepithelial CD4+ T cells controls gut inflammation. Science. 2016 Jun 2. pii: aaf3892.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CD4#
40
#炎症反应#
27
#SCIE#
34
#肠道炎症#
29
science精品啊
72
值得研究
156