JAMA Neurology:新发现:美国科学家首次发现一种新基因,有望治疗阿尔茨海默症
2020-06-25 转化医学网 转化医学网
近日,哥伦比亚大学欧文医学中心的研究人员发现一种新基因,这种新基因可能是大脑首次出现淀粉样蛋白板块的原因,这一发现有望为阿尔茨海默症带来新疗法。
根据哥伦比亚大学欧文医学中心的研究人员领导的一项研究,一种新发现的阿尔茨海默症基因(RBFOX1)可能导致大脑中首次出现淀粉样蛋白斑块。
RBFOX1基因的一些变体似乎增加了构成这些斑块的蛋白质片段的密度,并可能导致神经元之间关键连接的破坏(阿尔茨海默症的另一个早期征兆)。
这一发现可能会带来阿尔茨海默症的新疗法,以及更好地识别出最有可能患上该病的人。
这项研究在6月22日发表在《美国医学会神经病学杂志》(JAMA Neurology)上,题为“Association Between Common Variants in RBFOX1, an RNA-Binding Protein, and Brain Amyloidosis in Early and Preclinical Alzheimer Disease”。
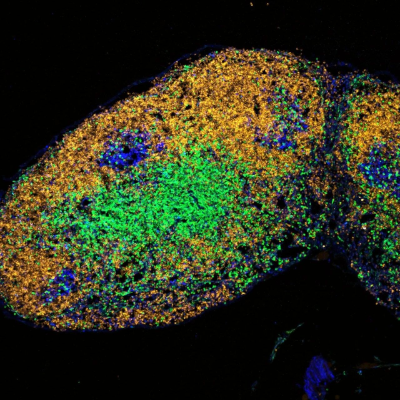
最近的几年中,淀粉样PET脑成像帮助揭示了阿尔茨海默症的早期标志,即脑中的淀粉样沉积。脑中淀粉样沉积在阿尔茨海默症出现明显症状之前的10年或15年就出现了。
但除了少数罕见的遗传基因导致的病例外,研究人员一直在寻找阿尔茨海默症患者大脑中淀粉样蛋白过度累积的原因。但人们在还没有出现阿尔茨海默症的症状之前,他们的大脑中就已经有淀粉样蛋白的沉积了。
哥伦比亚大学瓦格罗斯内科医生、外科医生学院的神经学主席、领导这项研究的理查德·马斯(Richard Mayeux)博士表示,“通过研究出现阿尔茨海默症最早标志的人,我们能够发现与疾病开始相关的基因。所有的这些基因很可能有助于找出阻止阿尔茨海默症的治疗方法。”
该研究调查了近4300名没有患阿尔茨海默症的人的基因组,但他们的大脑中已经包含了可变数量的淀粉样斑块,这是通过淀粉样示踪剂的PET成像技术来测量的。
一项基因分析发现了淀粉样蛋白沉积、载脂蛋白-e(APOE)(一种已知的阿尔茨海默症基因)和一种新基因RBFOX1之间的联系。在研究中(主要是欧洲血统的人)大约有10%的人出现了RBFOX1的变异,这与淀粉样蛋白沉积的出现有关。
大脑中RBFOX1含量的降低似乎与生活中淀粉样蛋白的增加和整体认知能力的下降有关。
确切地揭示RBFOX1是如何调节淀粉样蛋白斑块的,有助于找出防止斑块积累的方法。早前的研究已经表明,RBFOX1与淀粉样前体的形成和神经元间突触的破坏有关。
RBFOX1和淀粉样斑块之间的联系可能相对容易理解,不像众所周知的APOE4和淀粉样蛋白之间的联系,在研究几十年后仍然不清楚。
马斯表示,“我们能够找到最终疾病的标记物是对抗阿尔茨海默症的真正进展。在症状出现的时候来改变疾病进程几乎是不可能的,因为到那时的话,疾病已经存在了10到15年。如果我们能够靶向产生淀粉样蛋白的基因,并以某种方式纠正这些问题的话,我们可能就能够预防这种疾病。”
原始出处:
Neha S. Raghavan, et al. Association Between Common Variants in RBFOX1, an RNA-Binding Protein, and Brain Amyloidosis in Early and Preclinical Alzheimer Disease. AMA Neurol. Published online June 22, 2020. doi:10.1001/jamaneurol.2020.1760.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阿尔茨#
32
#Neurol#
33
#阿尔茨海#
41
#新发现#
35
#阿尔茨海默#
26
#新基因#
38
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
58
#阿尔茨海默氏症#像这种突变体,应该是具有治疗潜力的如果开发新药应该有望能成功,这样老年痴呆的治疗就进入了靶向治疗时代
131