贝伐珠单抗治疗肺癌脑转移伴难治性瘤周水肿的不良反应
2021-11-20 MedSci原创 MedSci原创
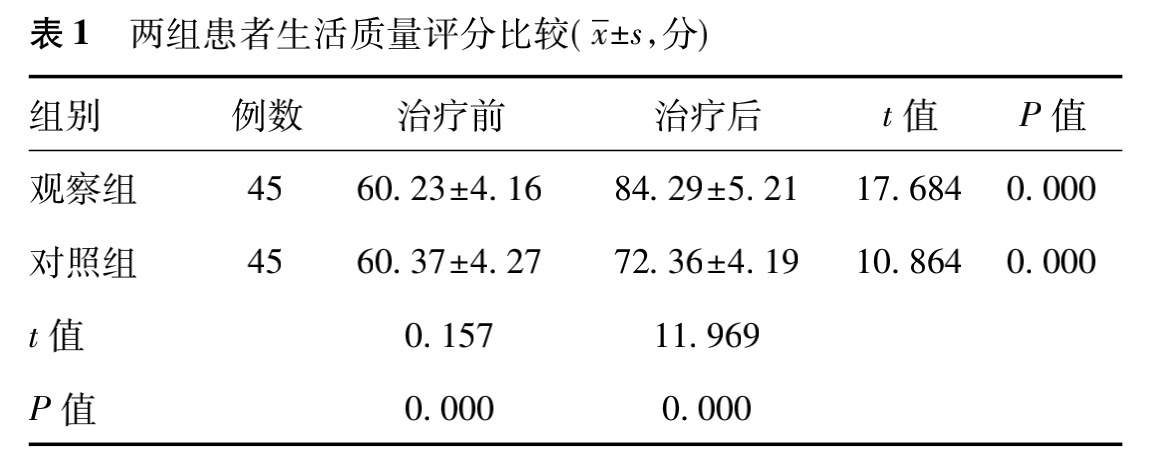
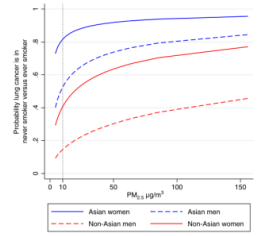
肺癌患者中脑转移是常见的死亡原因,发生率较高,自然 病程低于 3 个月。瘤周水肿的常规治疗手段为脱水及激素治疗,但由于血脑屏障原因,很多化疗药物无法实现良好的治疗效果。目前肺癌脑转移主要采取替莫唑胺、
肺癌患者中脑转移是常见的死亡原因,发生率较高,自然 病程低于 3 个月。瘤周水肿的常规治疗手段为脱水及激素治疗,但由于血脑屏障原因,很多化疗药物无法实现良好的治疗效果。目前肺癌脑转移主要采取替莫唑胺、卡氮芥类药物治疗,虽具有一定效果,但起效速度较慢。
本次研究对象是2017年8月~2018 年7月收治的 90 例肺癌脑转移的伴瘤周水肿患者,采用计算机随机法将其分为两组,每组各 45 例。观察组男 25 例,女 20 例,年龄 34 ~ 76 岁,平均( 55. 23±3. 42) 岁; 对照组男 24 例,女21例,年龄 33~75 岁,平均( 54. 29±3. 16) 岁。对两组研究对象基线资料比较,差异无统计学意义( P>0. 05) ,有可比性。
对照组采取常规治疗,给予地塞米松,初始药物剂量 0.75~3 mg,4 次/d,之后1片/d,药物剂量为0. 75 mg,依据患者实际病情进行有效调整,并给予静脉滴注甘露醇。与此同时,患者接受放疗与化疗。②观察组给予贝伐珠单抗治疗; 贝伐珠单抗的药物剂量为 5 mg /kg,用药间隔时间为 2 ~ 3 周。对于贝伐珠单抗联合全身化疗患者,应每间隔 3 周,进行 1 次给药。与放疗患者联合,需在放疗前给予 1 次用药,为减轻放射性脑损伤及单纯减轻脑水肿,用药间隔2~3周,需依据患者实际病情,决定用药情况。观察指标: ①对比两组患者治疗前后生活质量评分: 运用生活质量评分表( KPS) 评估患者治疗前后生活情况。②对比两组患者治疗总有效率: 显效: 临床症状完全消失,无不良反应; 有效: 临床症状基本消失,存在轻度不良反应; 无效: 没有消失临床症状,不良反应情况明显。总有效率 = ( 显效+有 效) ÷总例数×100% 。③对比两组患者不良反应情况。
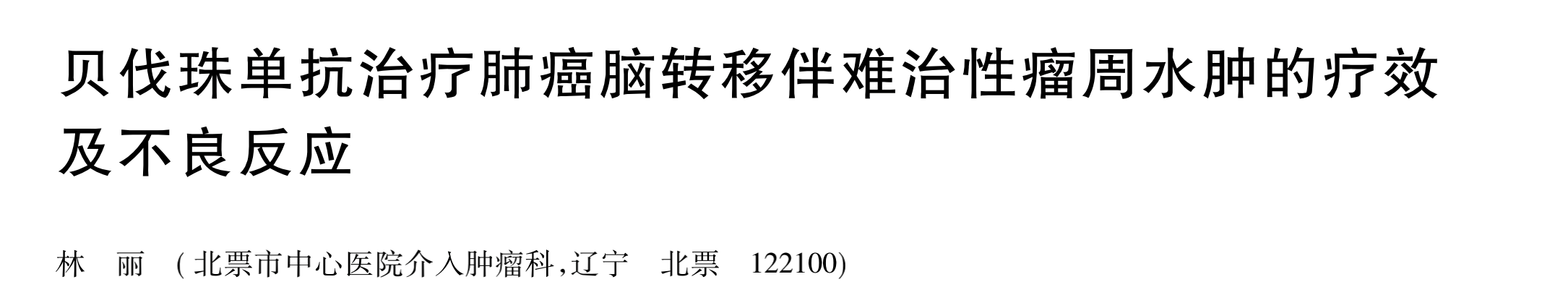
两组生活质量评分比较: 治疗前,两组患者生活质量评分差异无统计学意义( P>0. 05) ; 治疗后,观察组生活质量评分更高,组间差异有统计学意义( P<0. 05) 。见表 1。
两组不良反应情况比较: 对照组患者发生痰中带血4例,鼻腔出血5例,便血2例,胃部不适3例,高血压2例; 观察组患者发生痰中带血5例,鼻腔出血4例,便血3例,胃部不适2例,高血压3例; 两组均未出现严重不良反应,相关症状经对症治疗后消失。对照组不良反应发生率 35. 56% ( 16/45)和观察组的 37. 78% ( 17 /45) 相近,差异无统计学意义( χ2 = 0. 892,P>0. 05) 。
近年来,随着广大医务工作者的深入研究,贝伐珠单抗在原发性脑瘤治疗方面日益成熟,经头颅MRI 证实,贝伐珠单抗在放化疗期间会明显缩小瘤周水肿及肿瘤,缩短和缓解患者恶心、疼痛等症状,提升持续治疗效果时间,增加病灶部位药物敏感性。但需要引起注意的是,贝伐珠单抗使用剂量过大可引发患者发生出血死亡情况,因此,在药物使用过程中,考虑药物不良反应的同时还需重视用药剂量。
综上所述,对肺癌脑转移伴难治性瘤周水肿患者采取贝伐珠单抗治疗效果确切,能够有效提升患者生活质量,降低不良反应,具有临床推广价值。
原始出处:
吉林医学 2021 年 2 月第 42 卷第 2 期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#贝伐珠#
25
#不良反应#
42
#水肿#
30
#贝伐#
25
#难治性#
28