Science:组蛋白单点突变可导致罕见儿童癌症
2016-05-16 佚名 生物谷
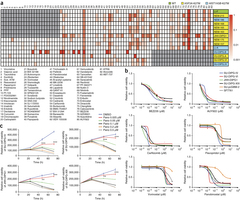
近日,国际学术期刊Science发表了一项最新研究进展,他们发现一种组蛋白编码基因发生缺陷与儿童恶性肿瘤的发生有关。来自美国威斯康星麦迪逊大学的Peter W. Lewis表示,大多数癌症的发生需要多个突变的共同作用,而他们发现的这个基因突变本身就足以导致形成肿瘤。组蛋白除了用于形成核小体,帮助进行基因组的压缩包装,还在基因的激活和沉默过程中发挥重要作用。有研究发现一些儿科肿瘤中包含高频的组蛋白H
近日,国际学术期刊Science发表了一项最新研究进展,他们发现一种组蛋白编码基因发生缺陷与儿童恶性肿瘤的发生有关。来自美国威斯康星麦迪逊大学的Peter W. Lewis表示,大多数癌症的发生需要多个突变的共同作用,而他们发现的这个基因突变本身就足以导致形成肿瘤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












拜读,好文
56
#单点突变#
48
#SCIE#
28
#组蛋白#
39
#罕见#
36
#儿童癌症#
38
学了了,不错的东西
117