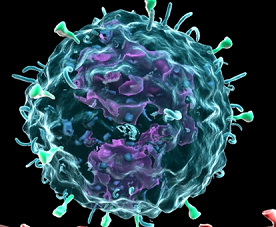
Immunity:呼吸道记忆CD4 T细胞抵抗病毒感染机制
2016-06-28 佚名 生物谷
说到冠状病毒,大家想必都不陌生。十几年前我国爆发的“非典型肺炎(SARS)”以及最近流行的“中东呼吸道综合征(MERS)”都是由冠状病毒引起的。冠状病毒的爆发似乎是不可避免的事情,因此,找到有效的广谱性疫苗成为解决该类型疾病的主要方式。目前大多数冠状病毒疫苗的原理都是针对模式株的糖基化蛋白引发抗体保护反应,这一方式一方面难以覆盖不断变异的野生病毒;另外,通过注射疫苗引发的抗体保护反应有效期都很有限
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Immunity#
0
#CD4#
32
关注值得,学习。赞!好文探究。
1
#呼吸道#
25
#抗病毒#
30