ANN SURG:腹腔镜与开腹结直肠癌切除术后腹腔粘连的比较
2018-03-27 MedSci MedSci原创
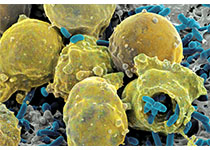
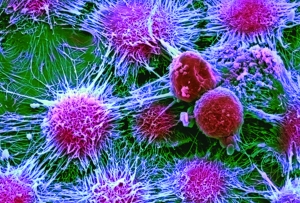
结直肠手术后,大部分患者均会出现粘连。腹腔镜似乎有助于减少粘连形成,但尚缺乏证据。比较开腹和腹腔镜结直肠手术的临床试验未评估过粘连形成的问题。ANN SURG近期发表了一篇文章,比较腹腔镜和开腹结直肠肿瘤切除术后粘连形成情况。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#结直肠癌切除术#
42
#切除术#
27
#腹腔粘连#
37
学习了.谢谢作者分享!
54
学习了.谢谢作者分享!
63
学习
48
#腹腔镜#
25
#结直肠#
26
谢谢分享.学习了
44
腹腔镜创伤小.易愈合
55