JNNP:7TPC-MRA评估CADASIL患者豆状动脉血流速度
2021-10-08 MedSci原创 MedSci原创
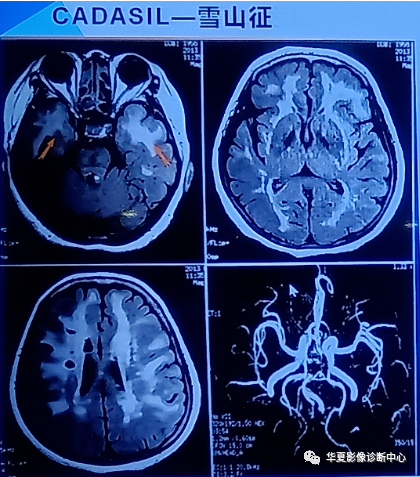
CADASIL(cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy)即
CADASIL(cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy)即是常染色体显性遗传病合并皮质下梗死和白质脑病。伴有皮质下梗死和白质脑病的常染色体显性遗传性脑动脉病,是一种遗传性小动脉疾病,位于19号染色体上的Notch3基因突变所致的遗传性脑小血管疾病,表现为皮质下缺血事件,并导致进行性痴呆伴假性球麻痹。
先前的研究报道,伴有皮质下梗死和白质脑病(CADASIL)的常染色体显性遗传性脑动脉病患者出现脑灌注不足。作为一种脑小血管疾病,脑小动脉血流速度降低可能先于脑灌注不足和病变形成。由于空间分辨率的限制,传统方法无法检测脑小血管的速度。超高MRI为我们研究CADASIL患者豆状突动脉(LSA)的速度提供了一种非侵入性方法。评估小动脉的血流速度可以在患者的长期随访中监测疾病的进展。本文发表在《神经病学,神经外科学和精神病学杂志》上()。
于2019年9月至2020年9月在北京大学第一医院登记了32名CADASIL患者和34名健康对照。登记了受试者选择、临床评估、MRI采集和分析的详细信息。磁共振血管造影(PC-MRA)在7T高分辨率(0.35×0.35×0.40)MR扫描仪上获得 ;使用低速编码(VENC)值(15.00cm/s)测量lsa的血流速度。LSA速度分析包括:(1)强度偏差校正;(2) 最大强度投影图像;(3) 基于阈值的降噪;(4) 利用相位差数据重构速度分量;(5) 提取LSA并计算平均速度。
一名患者和三名健康对照者因过度的头部运动导致较大的伪影和较差的图像质量而被排除在外。最终,在本研究中纳入了来自24个家庭的31名患者和31名健康对照者。在所有这些CADASIL患者中,12例mRS评分异常,9例Barthel指数异常。在26名接受焦虑和抑郁评估的患者中,13名汉密尔顿焦虑量表(HAMA)得分异常,17名汉密尔顿抑郁量表(HAMD)得分异常。在这26名接受MMSE认知评估的患者中,9名MMSE评分异常。在22名患者中,7名接受Montrealcognitive Assessment(MoCA)评估的患者得分异常。
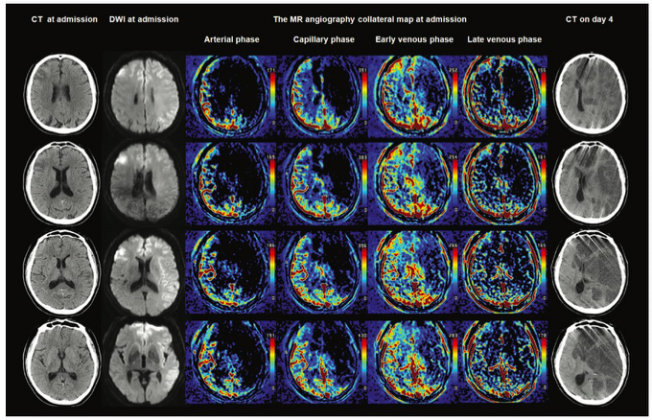
不同研究组组的代表性速度图。(A)有症状的CADASIL患者,(B)年龄匹配和性别匹配的无症状NOTCH3致病性变体携带者,(C)年龄匹配和性别匹配的健康对照组的代表性病例。VLSA,豆状动脉的血流速度。
与对照组(11.75±1.07 cm/s)相比,CADASIL组的LSA血流速度较低(10.04±1.82 cm/s)(p<0.001)。此外,无症状携带者LSA的血流速度(11.47±1.55 cm/s)显著高于有症状患者(9.45±1.60 cm/s)(p=0.003),而与健康对照组相似(p=0.543)。此外,CADASIL患者的LSA数量与对照组无差异(p=0.681)。结果显示LSA的速度随着年龄的增长而显著降低。LSA的速度与异常mRS评分显著相关。
通过7T的PC-MRA检查,首次在CADASIL患者中发现LSA血流速度显著降低。此外,LSA中的血流速度可用于评估疾病的严重程度,因为它与患者的临床和MRI特征相关。7T的PC-MRA得益于超高场中更高的对比度和更高的空间分辨率。LSA可在有或无VENC梯度的图像中清晰识别。高分辨率和低VENC保证了常规方法无法检测的慢流速度定量的准确性。在CADASIL患者中观察到LSAs中的血流速度显著降低,这可能是MCAs中毛细血管灌注和血流速度异常变化的原因。
在未来的研究中,需要采用先进的加速成像技术,实现时间分辨速度测量或具有高分辨率和足够空间覆盖的更短扫描时间,但是目前无法实现的。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#血流速度#
39
#CADASIL#
37
#动脉血流#
46
#动脉血#
43
#ADA#
31
#MRA#
30