别再让急性心梗患者盲目吸氧了!
2016-08-08 光啊啊 医学界心血管频道
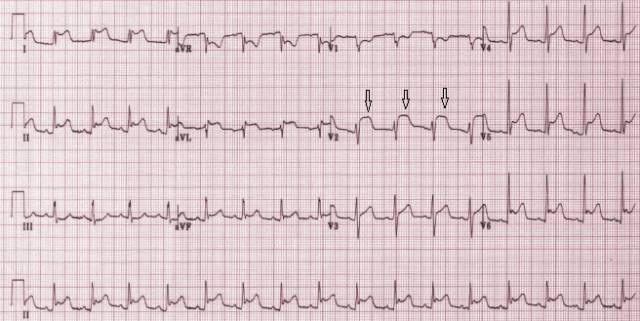
STEMI患者氧疗的历史很悠久,一个世纪前(1900年)Steele首次提出对严重心绞痛患者给予吸氧,1930年Levy和Barach给予4例AMI患者吸氧,发现临床症状有所改善。其后的几十年,临床医生一般会对就诊的急性心肌梗死(AMI)患者常规给予吸氧治疗。吸氧一直被认为可增加动脉血氧含量,改善缺血心肌的氧供给,减少心肌梗死的面积。事实上,氧气不仅是一种气体,也是一种血管活性物质,因此在不缺氧的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心梗患者#
41
学习了,好
63
值得学习
65
有待进一步研究
55
有待进一步研究
58
好好学习
61
继续关注
33
继续学习
34
#急性心梗#
45