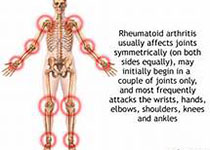
类风湿关节炎相关性间质性肺疾病1例
2018-04-28 雷盼 吴昊泽 李亚亭 湖北医药学院学报
患者,女,58岁,患者8h前无明显原因突发剧烈头痛,伴恶心、呕吐,急于当地县医院行头颅CT:蛛网膜下腔出血,为进一步治疗,转至本院。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相关性#
31
#关节炎#
35
#类风湿#
34
#间质性肺疾病#
39
#风湿关节炎#
25
#间质性#
24
好文献学习了
40
学习了
39
学习了.谢谢分享.
36