J Am Acad Dermatol:使用靶向抗癌药物能促进患者的色素改变(Meta分析)
2017-09-19 MedSci MedSci原创
背景和目的:信号网络的发现推动了致癌过程的研究,导致了靶向抗癌药物的发展。而这些药物的色素性不良事件是未知的。因此来自美国的研究人员已发表的临床试验进行了系统回顾和荟萃分析,旨在确定靶向治疗引起的色素改变进展的发生和风险。
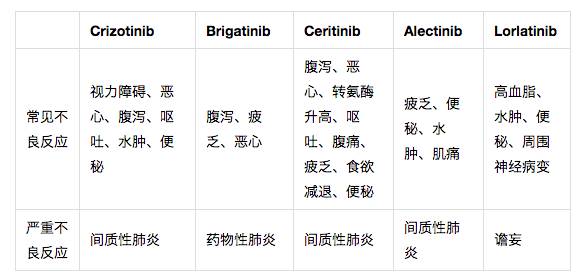
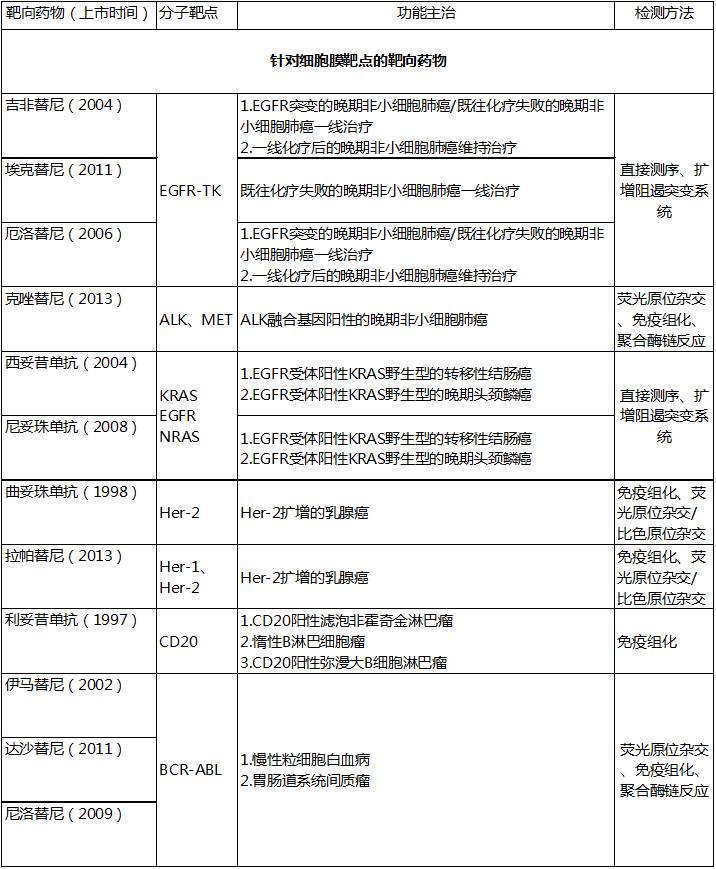
背景和目的:信号网络的发现推动了致癌过程的研究,导致了靶向抗癌药物的发展。而这些药物的色素性不良事件是未知的。因此来自美国的研究人员已发表的临床试验进行了系统回顾和荟萃分析,旨在确定靶向治疗引起的色素改变进展的发生和风险。方法:研究人员通过综合搜索确定靶向治疗引起色素改变的研究报告,并计算了发病率和相对风险。研究人员通过回顾病例报告和病例系列分析了解临床特点。结果:研究人员共检索到了36个临床试验,包括8052例患者。癌症靶向治疗导致的在皮肤和头发部位的所有等级的色素改变的总体发病率分别为17.7%(95%置信区间[CI],11.9-25.4)和21.5%(95% CI,14.9-30.1)。在皮肤和头发部位的所有等级的色素改变的相对风险为93.7(95% CI,5.86-1497.164)和20.1(95% CI,8.35-48.248)。在53例病例报道/病例系列分析(n = 75例),表皮生长因子受体和BCR/ABL抑制剂是最常见的致病因素。局限性:肿瘤科医生报告这些事件时存在潜在的漏报和变异性可能。结论:本研究的结果的表明靶向抗癌治疗过程中的色素改变进展存在重大风险。适当的咨询
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ACA#
32
#靶向抗癌#
0
#色素#
21
#MET#
24
#Meta#
28
#靶向抗癌药物#
29
#抗癌药物#
26
#抗癌药#
22