JAMA Cardiology:NBA球员的心脏有啥不一样?
2016-02-25 yinghao 译 MedSci原创
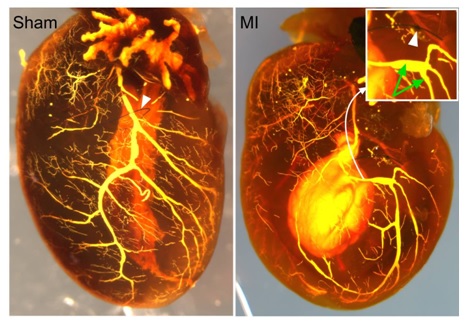
从字面的定义来看,职业篮球运动员指的是一群比我们更高、更壮、也更加体能充沛的人。实际上,他们的心脏和我们相比,也有着不为人知的区别。与其他运动员相比,美国的篮球运动员突发心脏病造成的死亡率远高于其他类型的疾病。但是,众所周知,随着长期的体育运动锻炼,心脏会发生一定的变化,变得更大、更重、也会更厚。因此对于这群更加高大的运动员群体,其心脏已经与常人相比出现了一定的改变,我们对其突发心脏病风险的认识还
原始出处:
David J. Engel, MD; Allan Schwartz, MD; Shunichi Homma, MD, Athletic cardiac remodeling in US professional basketball players. JAMA Cardiology, 2016.2.24.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cardiology#
39
#Cardiol#
21
好几个熟悉的名字
96
非常好的研究
130
有点意思
125
有意思
115
当然
114
有道理
69
有道理
110
适可运动是好
134