ANN ONCOL:Nintedanib治疗难治性转移性结直肠癌
2018-09-28 MedSci MedSci原创
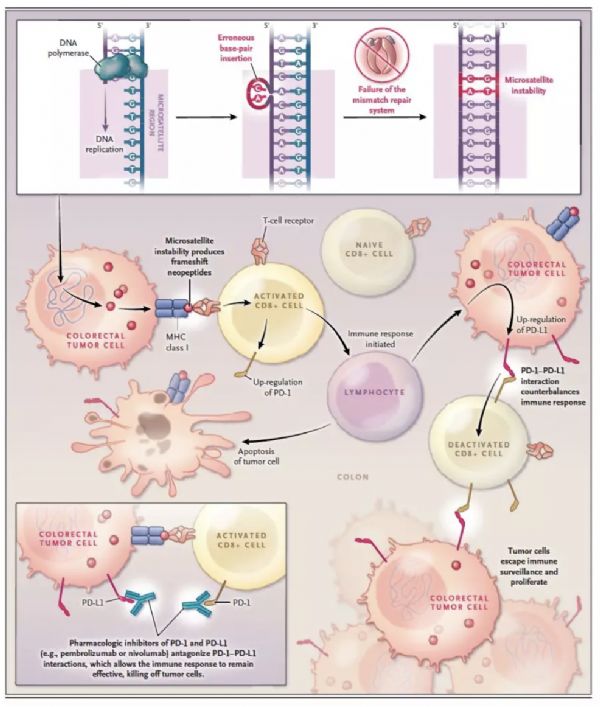
血管生成对结直肠癌(CRC)生长和转移至关重要。I / II期临床研究证实了nintedanib(一种血管激酶抑制剂)对转移性CRC患者具有疗效。ANN ONCOL近期发表了一篇文章,报道了nintedanib治疗接受标准疗法失败后的难治性CRC患者的有效性和安全性。
原始出处:
E Van Cutsem , T Yoshino, et al. Nintedanib for the treatment of patients with refractory metastatic colorectal cancer (LUME-Colon 1): a phase III, international, randomized, placebo-controlled study. ANN ONCOL.September 2018 doi: https://doi.org/10.1093/annonc/mdy241
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
30
#TED#
33
#Nintedanib#
37
#转移性#
23
#结直肠#
40
#难治性#
37
学习一下,谢谢分享!
54
学习了
66