Eur Heart J:睡眠呼吸暂停的低氧负担可预测心血管疾病相关死亡率
2018-10-30 xing.T MedSci原创
由此可见,“低氧负担”是一项来自夜间睡眠研究的易于推断的指标,可预测人群的CVD死亡率。研究结果表明不仅仅是频率而且与睡眠相关的上呼吸道阻塞的深度和持续时间是重要的疾病特征。
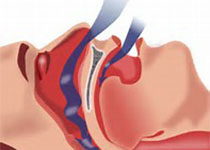
呼吸暂停-低通气指数(AHI)是睡眠呼吸暂停严重程度的常见临床指标,其很难预测睡眠呼吸暂停的不良结局,可能是因为AHI不能充分捕捉疾病负担。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员试图评估通过“低氧负担”量化睡眠呼吸暂停的严重程度是否可以预测40岁及以上成年人的死亡率。
这些样本来自两项队列研究:老年人睡眠障碍结局(MrOS)研究(其纳入了2743名男性,年龄为76.3±5.5岁)以及睡眠心脏健康研究(SHHS)(其纳入了5111名中老年人,52.8%为女性,年龄为63.7±10.9岁)。结局是全因和心血管疾病(CVD)相关的死亡率。通过测量来自事件前基线的去饱和曲线下与呼吸事件相关面积来确定缺氧负荷。Cox模型用于计算缺氧负荷的调整后风险比。
与AHI不同,低氧负担可预测CVD死亡率,但不能预测全因死亡率。在MrOS研究中具有低氧负荷最高的两个五分位数的个体的风险比分别为1.60[95%置信区间(CI)为1.13-2.28]和2.04(95%CI为1.34-3.09)。同样,在SHHS研究中最高五分位数低氧负荷组的风险比为1.96(95%CI为1.11-3.43)。
由此可见,“低氧负担”是一项来自夜间睡眠研究的易于推断的指标,可预测人群的CVD死亡率。研究结果表明不仅仅是频率而且与睡眠相关的上呼吸道阻塞的深度和持续时间是重要的疾病特征。
原始出处:
Ali Azarbarzin.et al.The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J.2018. https://doi.org/10.1093/eurheartj/ehy624
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#睡眠呼吸#
27
#ART#
42
#血管疾病#
42
#HEART#
36
#呼吸暂停#
45
谢谢分享,学习一下。
54
学习了,谢谢分享。
59