JCEM:依帕列净可以改善2型糖尿病患者的β细胞的功能?
2018-01-14 MedSci MedSci原创
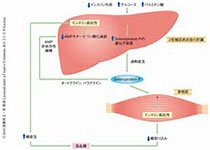
2018年1月12日在JCEM上发表的一篇文章旨在研究使用依帕列净(SGLT2抑制剂)降低血糖浓度能否改善T2DM患者β细胞的功能。
2018年1月12日在JCEM上发表的一篇文章旨在研究使用依帕列净(SGLT2抑制剂)降低血糖浓度能否改善T2DM患者β细胞的功能。
研究人员纳入了15例T2DM患者,并接受依帕列净(25mg/d)治疗2周,用9步高血糖钳夹(每步=+40mg/dl)在依帕列净治疗前、之后48h和14周测定β细胞的功能。
研究结果显示依帕列净在第1天和第14天分别引起101±10和117±11克的糖尿,分别使空腹血糖下降低了25±6和38±8 mg / dl(两者均p <0.05)。在依帕列净开始后48小时和14天(两者均p <0.01),增加了血浆C肽浓度曲线下的增量面积,分别为48±12%和61±10%。在第3天和第14天进行的高血糖钳夹时,依帕列净也导致葡萄糖输注速率增加,与基线相比分别增加了15%和16%(均p <0.05)。 依帕列净开始48小时和14天后,β细胞功能(以胰岛素分泌/胰岛素抵抗(IS / IR)指数测量)增加了73±21%和112±20%(均为p <0.01)。 依帕列净也在48小时和14天后分别使高血糖钳夹的β细胞葡萄糖敏感性增加了42%和54%(均为p <0.01)。
由上述研究结果可以发现依帕列净降低T2DM血浆葡萄糖浓度:(1)增加β细胞葡萄糖敏感性;(2)改善β细胞功能(IS / IR指数)。
原始出处:
Hussein Al Jobori.et al. Empagliflozin Treatment is Associated with Improved Beta Cell Function in T2DM. J Clin Endocrinol Metab. 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCEM#
40
#JCE#
0
学习了.谢谢.
69
#2型糖尿病患者#
34
#依帕列净#
45
#糖尿病患者#
19
#β细胞#
40