Heart:先心病患儿的很大摄氧量要明显低于正常对照儿童
2017-11-24 MedSci MedSci原创
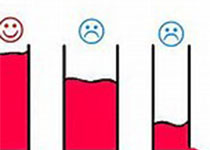
本研究的目的旨在比较评估先天性心脏病患儿的心肺功能与性别、年龄匹配的正常儿童心肺功能的差异,并探究影响先心病患儿最大摄氧量(VO2max)的临床因素。本次横断面多中心临床研究纳入了496名先心患儿和302名正常对照,这些对象均接受了全面的心肺功能评估(CPET)。先心组患儿的平均VO2max与对照组平均VO2max值分别是预测值的93%±20% 和 107%±17%,VO2max在先心病组明显更低
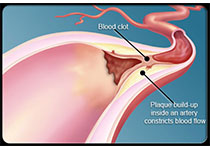
本研究的目的旨在比较评估先天性心脏病患儿的心肺功能与性别、年龄匹配的正常儿童心肺功能的差异,并探究影响先心病患儿最大摄氧量(VO2max)的临床因素。本次横断面多中心临床研究纳入了496名先心患儿和302名正常对照,这些对象均接受了全面的心肺功能评估(CPET)。先心组患儿的平均VO2max与对照组平均VO2max值分别是预测值的93%±20% 和 107%±17%,VO2max在先心病组明显更低(37.8±0.3vs 42.6±0.4mL/kg/min, P<0.0001),每年VO2max值的下降值在先心病组中也更高(-0.84±0.10vs -0.19±0.14mL/kg/min/年, P<0.01),其中在男孩中为-0.72±0.14vs 0.11±0.19 mL/kg/min/年, P<0.01,女孩为-1.00±0.13 vs -0.55±0.21 mL/kg/min/年, P=0.05。经多元分析后,与VO2max相关的临床因素有:体重指数(BMI)、通气性无氧阈、女性、限制性通气障碍、右室收缩性高血压、三尖瓣关闭不全、心脏导管或手术次数、以及存在的遗传
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#对照#
28
#先心病#
27
#ART#
36
#HEART#
24
学习了.涨知识
70