NEJM:脓毒症紧急护理期间治疗时间与死亡率有何关系?
2017-05-22 xing.T MedSci原创
由此可见,脓毒症患者较快的完成3小时捆绑措施和更早的接受抗生素治疗都与较低的调整后的住院死亡率风险相关,而与快速完成静脉输液无关。
2013年,纽约开始要求医院遵守早期识别和治疗脓毒症的协议。然而,对于脓毒症的快速治疗是否能改善患者的预后仍存在争议。最近,顶级医学期刊NEJM上针对这一问题发表了一篇研究文章。
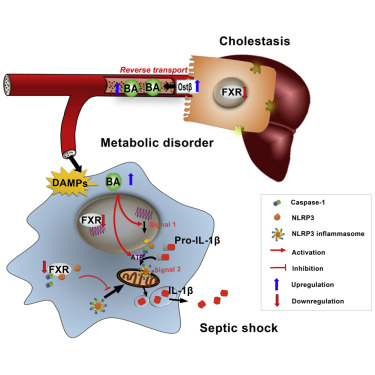
研究人员分析了从2014年4月1日到2016年6月30日期间纽约卫生部报告的脓毒症和感染性休克患者的数据。这些患者在到达急诊6小时内启动了脓毒症协议,并在12小时内完成了脓毒症患者3小时捆绑措施的所有项目(即,血培养、广谱抗菌剂和乳酸测量)。多层次的模型被用来评估完成3小时捆绑措施的时间与风险调整后的死亡率之间的相关性。研究人员还评估了给予抗生素和完成初始静脉注射液体的时间。
在149家医院的49331例患者中,40696名患者(82.5%)在3小时内完成3小时捆绑措施。完成3小时捆绑措施的中位时间为1.30个小时(四分位距为为0.65-2.35),给予抗生素的中位时间为0.95个小时(四分位距为0.35-1.95),完成静脉注射液体的中位时间为2.56小时(四分位距为1.33-4.20)。在12小时内完成3小时捆绑措施的患者中,完成捆绑措施的时间越长,调整后的住院死亡率风险更高(比值比为每小时1.04;95%可信区间[CI]为1.02-1.05;P<0.001),给予抗生素治疗的时间越长也是一样的(比值比为每小时1.04;95%CI为1.03-1.06;P<0.001),而与完成初始静脉注射液体的时间越长无关(比值比为每小时1.01;95%CI为0.99-1.02;P=0.21)。
由此可见,脓毒症患者较快的完成3小时捆绑措施和更早的接受抗生素治疗都与较低的调整后的住院死亡率风险相关,而与快速完成静脉输液无关。
原始出处:
Christopher W. Seymour, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis.NEJM.2017.http://www.nejm.org/doi/full/10.1056/NEJMoa1703058?query=featured_home
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#治疗时间#
24
#紧急#
22
学习
85
学习
87