Crit Care Med:脓毒症相关的30天风险标准化再住院率
2017-05-07 MedSci MedSci原创
近期,一项发表在杂志Crit Care Med上的研究旨在确定脓毒症存活者之间的再入院率,医院之间的差异变化,并确定质量检测是否与脓毒症患者再入院时的表现相关。此项研究为自2008年至2011年在医疗保险费用服务数据库中选取脓毒症再入院患者的横断面研究。研究者们评估了脓毒症生存者的医院级别、风险标准化、30天的再入院率,并比较了区域、所有权、教学状况、败血症数量、医院规模以及服务不足的患者比例。研
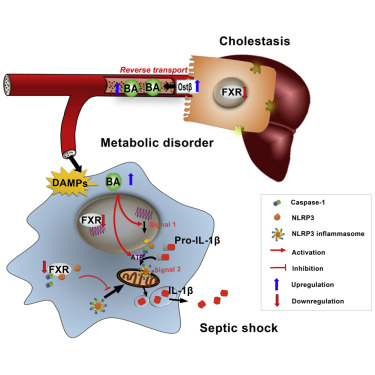
近期,一项发表在杂志Crit Care Med上的研究旨在确定脓毒症存活者之间的再入院率,医院之间的差异变化,并确定质量检测是否与脓毒症患者再入院时的表现相关。
此项研究为自2008年至2011年在医疗保险费用服务数据库中选取脓毒症再入院患者的横断面研究。
研究者们评估了脓毒症生存者的医院级别、风险标准化、30天的再入院率,并比较了区域、所有权、教学状况、败血症数量、医院规模以及服务不足的患者比例。研究者们检查了风险标准化再入院率与医院水平复合质量和死亡率的关系。
从2008年至2011年的3315家医院中,共633,407例患者住院治疗,中位风险标准化再入院率为28.7%(四分位数间距26.1-31.9)。风险标准化再入院率存在着区域差别(东北,30.4%;南部,29.6%;中西部,28.8%;西部,27.7%; p <0.001),教学与非教育状况差异(31.1%vs 29.0%;p <0.001),服务不足最多的医院(30.6%vs 28.7%;p <0.001)。与表现最差的医院相比,复合质量测评中表现最好的医院的风险标准再入院率最高(32.0%vs 27.5%; p <0.001)。与死亡率最低的医院相比,死亡率最高的医院的风险标准再入院率较低(28.7%vs 30.7%; p <0.001)。
此项研究表明:三分之一的脓毒血症存活者重新入院,医院之间存在广泛的差异。一些人口和结构因素与这种变化有关。高质量住院护理的措施与更高的再入院率相关。
原始出处:
Norman BC, Cooke CR, et al. Sepsis-Associated 30-Day Risk-Standardized Readmissions: Analysis of a Nationwide Medicare Sample. Crit Care Med. 2017 Apr 29. doi: 10.1097/CCM.0000000000002476.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标准化#
27
#再住院率#
38
#30天#
41
#Med#
37
学习了,涨知识了!!
51
学习,感谢分享!
43
学习了谢谢分享
43
不同医院的诊疗水平差距所导致
40
谢谢分享 学习了!
44
谢谢分享,谢谢
36