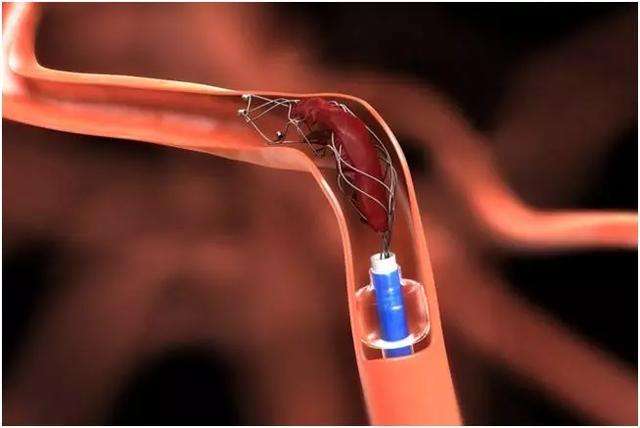
血管解剖弯曲是血栓切除失败的常见原因在弯曲的血管中,支架回收器(SRs)会被拉伸,在回收过程中可能会崩溃,从而导致与血栓失去相互作用。血管弯曲也减少了抽吸导管尖端与血栓的接触,并损害了血栓的抽吸弯曲降低了SR取栓和接触吸入(CA)导管的性能,增加了所需的设备通过次数,降低了实现完全再灌注的可能性。
虽然颈内动脉(ICA)迂曲在机械取栓时是一个重大的挑战,但很少有研究检查颈内动脉迂曲对机械取栓结果的影响。
Junpei Koge等在STROKE杂志刊发文章,研究了ICA弯曲度与MT预后之间的关系。

在一项以登记为基础的医院队列研究中,连续尝试机械取栓的前循环卒中患者被分为两组:颅外或海绵窦段颈动脉迂曲组(迂曲组)和非迂曲组(非迂曲组)。颅外段ICA弯曲被定义为存在盘绕或扭结。海绵窦段颈动脉迂曲由后膝后侧偏斜或类似simmons型导管的形状确定。结果包括首通效应(FPE;首次通过后延长脑梗死溶栓评分2c/3)、预后良好(3个月改良Rankin Scale评分0-2)、颅内出血。
结果如下
在370例患者中,124例为迂曲组(颅外ICA迂曲35例;海绵窦段颈动脉弯曲,70;两个部位都有弯曲,19)。
迂曲组比非迂曲组有更高比例的女性和心房纤颤。
在迂曲组中获得FPE的频率低于非迂曲组(21% vs 39%;调整后的优势比为0.45 [95% CI, 0.26-0.77])。

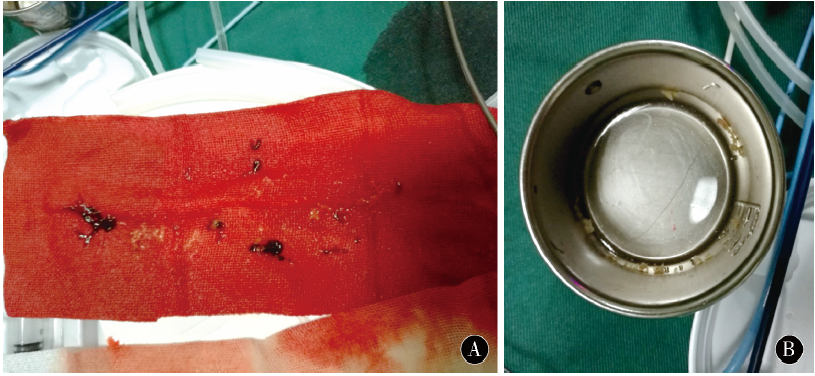
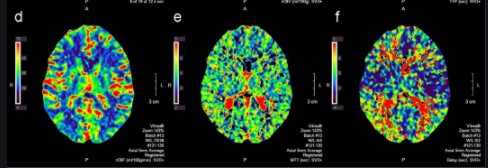
根据颈内动脉(ICA)迂曲位置的手术结果。根据ICA迂曲位置的结果显示(A)首次通过后的再灌注状态,(B)最终的再灌注状态,和(C)颅内出血。eTICI提示脑梗死患者溶栓时间延长
1. ICA曲度与脑梗死≥2b再灌注的患者从穿刺到延长溶栓时间的延长独立相关(β=23.19 [95% CI, 13.44-32.94])。各组之间的良好结果相似(46% vs 48%;P = 0.87)。
2. 颅内出血的频率(54% vs 42%;调整优势比为1.61 [95% CI, 1.02-2.53])和脑实质血肿(11% vs 6%;经调整的优势比(2.41 [95% CI, 1.04-5.58])在迂曲组中较高。
3. 在迂曲组中,接受联合支架取栓和接触吸入取栓术的患者的FPE率与单独接受这两种手术的患者相似(22% vs 19%;P = 0.80)。
4. 然而,在非迂曲组中,接受支架回收和接触吸入联合治疗的患者FPE发生率显著升高(52% vs 35%;P = 0.02)。

根据一线机械取栓策略的首通效应。(A)颈内动脉非迂曲组和(B)颈内动脉迂曲组中根据一线机械取栓策略的首通率
ICA迂曲与较低的FPE发生率和较高的MT后脑出血发生率独立相关。ICA迂曲对症状性脑出血及预后无显著影响。对于迂曲的ICA,没有观察到联合SR和CA的协同效应,目前所有MT策略中FPE的发生率同样低。为了改善MT的治疗结果,需要开发有希望治疗迂曲血管患者的设备和技术。
原文出处
Internal Carotid Artery Tortuosity: Impact on Mechanical Thrombectomy
https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.037904
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#取栓术#
55
#取栓#
52
#机械取栓#
45
#颈内动脉#
54