Br J Cancer:安罗替尼(Anlotinib):小细胞肺癌患者的三线或后续治疗药物
2021-05-23 xiaozeng MedSci原创
复发性小细胞肺癌(SCLC)的治疗一直是临床实践中的一大挑战。自1996年拓扑替康(topotecan)被批准为二线治疗药物后的近30年里,并没有药物显示出对SCLC足够的功效。
复发性小细胞肺癌(SCLC)的治疗一直是临床实践中的一大挑战。自1996年拓扑替康(topotecan)被批准为二线治疗药物后的近30年里,并没有药物显示出对SCLC足够的功效。
目前已经评估了许多针对复发性SCLC的治疗策略,但相关的临床获益仍有限。SCLC是一种高度血管化的肿瘤,现已在SCLC患者中评估了几种抗血管生成剂,但并未显示出良好的疗效。
安罗替尼(Anlotinib)不同于其他的多靶点抗血管生成剂。其能够抑制VEGFR1/2/3(血管内皮生长因子受体1/2/3)、FGFR1-4(成纤维细胞生长因子受体1-4)、PDGFR-α/β和c-Kit,并显示出对SCLC细胞系的潜在抑制作用。在2018年安罗替尼被美国国家药品管理局(NMPA)批准为NSCLC的三线治疗药物。
基于以上原因,该研究旨在评估安罗替尼单药治疗对SCLC患者的疗效和安全性。
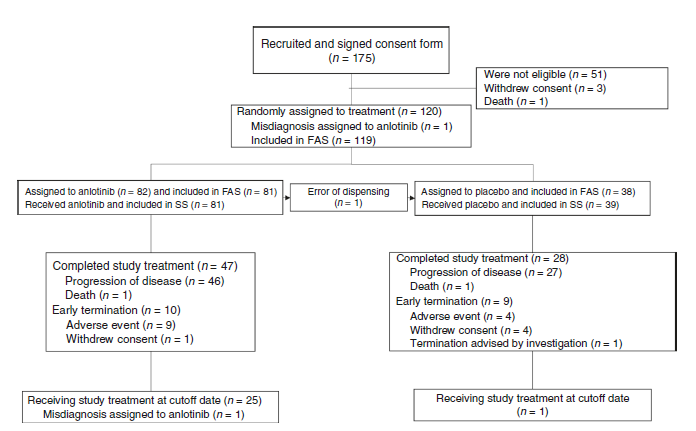
研究流程图
研究人员在中国的11家机构中进行了该2期试验。主要募集了经病理证实为SCLC且至少接受了两线化疗失败的患者。通过将受试者以2:1的比例进行随机分配,患者每3周为一个疗程,疗程中的14天进行每天一次口服12 mg安罗替尼或安慰剂治疗。试验的主要终点为患者的无进展生存期(PFS)。
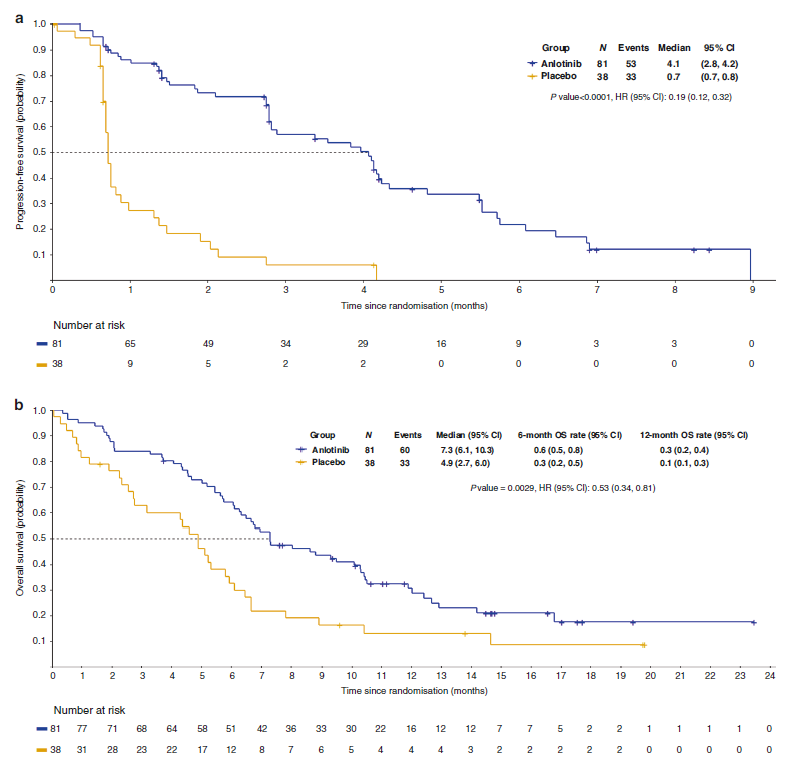
结果显示,在2017年3月30日至2018年6月8日之间,共有82例和38例患者被随机分配接受安罗替尼和安慰剂治疗。相比于安慰剂组,安罗替尼组患者的中位PFS显著更长(4.1个月对0.7个月)。安罗替尼组患者的总生存期(OS)显著长于安慰剂组(7.3个月对4.9个月)。
患者的无进展生存期和总生存期的Kaplan-Meier曲线
总而言之,对于中国SCLC患者,作为第三线或后续治疗药物的安罗替尼显示出了PFS和OS的改善,且安全性良好。
原始出处:
Cheng, Y., Wang, Q., Li, K. et al. Anlotinib vs placebo as third- or further-line treatment for patients with small cell lung cancer: a randomised, double-blind, placebo-controlled Phase 2 study. Br J Cancer (18 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗药物#
43
#肺癌患者#
42
学习
75
好文章!
65
学习到很多
63
很好
63