J Thorac Oncol:RovalPituzumab tesiine与拓扑替康用作小细胞肺癌二线治疗方案的疗效对比
2021-03-04 MedSci原创 MedSci原创
本研究旨在比较Rova-T和拓扑替康作为DLL3高表达的晚期或转移性小细胞肺癌的二线治疗的疗效和安全性
δ样蛋白3(DLL3)是一种非典型的Notch配体,在小细胞肺癌(SCLC)肿瘤中表达,且在正常成人组织中检测不到。RovalPituzumab tesiine(Rova-T)是一种DLL3靶向抗体与细胞毒剂吡咯洛苯二氮类药物相连的抗体-药物耦合物。
TAHOE是一项开放标签的随机3期研究,旨在比较Rova-T和拓扑替康(topotecan)作为DLL3高表达的晚期或转移性小细胞肺癌的二线治疗的疗效和安全性。
受试患者按2:1随机分成两组,分别接受Rova-T(0.3 mg/kg,静滴,42天一疗程,每疗程的第一天用药,共2个疗程,符合预定标准的患者可额外再接受2个疗程)或拓扑替康(1.5 mg/m2,静注,21天一疗程,第1-5天用药)。主要终点是总存活率(OS)。
共招募了444例患者:Rova-T组 296例、拓扑替康组 148例。中位年龄为64岁,77%的患者在最初确诊时已处于广泛期。
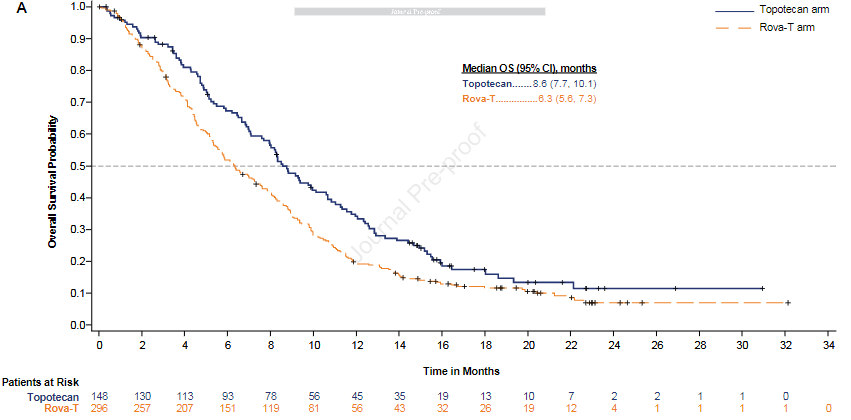
两组的总存活率
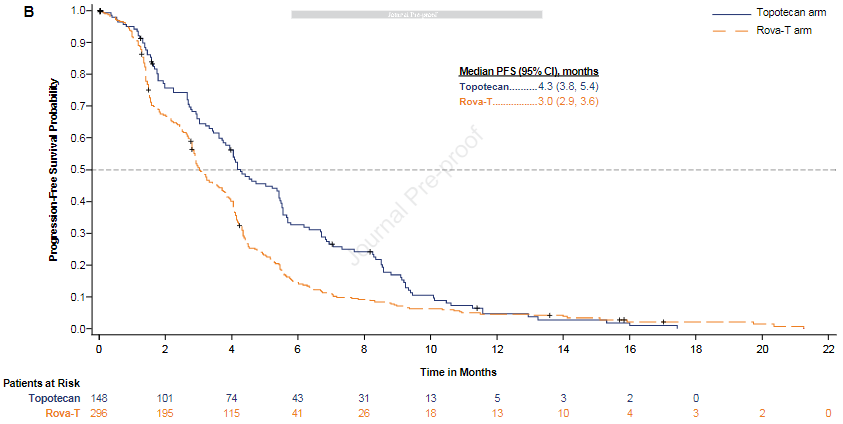
两组的无进展存活率
Rova-T组和拓扑替康组的中位OS(95%CI)分别为6.3个月(5.6-7.3)和8.6个月(7.7-10.1)(风险比 1.46 [95%CI 1.17-1.82])。鉴于观察到的Rova-T的OS较拓扑替康组的短,一个独立的数据监测委员会建议停止招募患者。这两种药物的安全性与既往报道的一致。
与目前标准的二线化疗方案拓扑替康相比,Rova-T在小细胞肺癌患者中表现出较差的OS,且有较高的浆膜腔积液、光敏反应和周围水肿发生率。
原始出处:
Blackhall Fiona,Jao Kevin,Greillier Laurent et al. Efficacy and Safety of Rovalpituzumab Tesirine Compared with Topotecan as Second-Line Therapy in DLL3-High Small Cell Lung Cancer: Results from the Phase 3 TAHOE Study. J Thorac Oncol, 2021, 10.1016/j.jtho.2021.02.009
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#THORAC#
42
#mAb#
39
#治疗方案#
38
#ALP#
39
#Oncol#
45
#二线治疗#
40
#ESI#
37
谢谢梅斯提供这么好的信息,学到很多
40
JTO上有很多不错的好文章,谢谢梅斯及时上新
44
谢谢梅斯分享这么多精彩信息
43