DIABETOLOGIA:原发性星形胶质细胞低糖复发后基础脂肪酸氧化增加
2019-04-04 不详 网络
<span style="font-size:12.0pt;font-family:宋体;mso-ascii-font-family: Calibri;mso-ascii-theme-font:minor-latin;mso-fareast-font-family:宋体;mso-fareast-theme-font: minor-fareast;mso-hansi-font-family:Ca
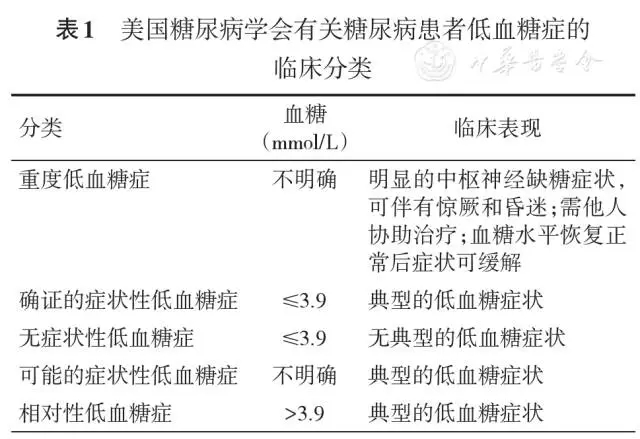
低血糖是1型糖尿病血糖控制的主要障碍。频繁的低血糖发作损害了对随后低血糖发作的意识。目前,关于支持低血糖意识的神经变化定义不清,且胶质细胞参与低血糖感知和葡萄糖调节的分子机制需要进一步研究。本研究的目的是探讨急性和复发性低血糖(RLG)是否改变人原发性星形胶质细胞(HPA)功能,以及通过何种机制改变HPA功能。
为了检测胶质细胞,特别是星形胶质细胞是否能检测到葡萄糖的变化,我们使用了HPA和U373星形细胞瘤细胞,并在体外将它们暴露于RLG中。这使得测量rlg相关的细胞代谢变化具有很高的特异性和敏感性。我们使用western blotting检测了蛋白磷酸化/表达的变化。利用海马细胞外通量分析仪评估代谢功能。采用免疫荧光成像技术检测细胞形态,采用酶法测定乳酸释放、糖原含量、细胞内ATP和核苷酸比值。
结果显示,amp活化蛋白激酶(AMPK)在病理生理相关的葡萄糖浓度范围内被激活。RLG在线粒体基础代谢过程中对脂肪酸氧化的依赖性增加,表现出线粒体应激的特征,包括质子泄漏增加和耦合效率降低。相对于葡萄糖利用率,低糖时乳酸释放增加,但未被RLG改变。RLG不影响基础糖摄取,对照组和RLG处理的细胞糖原水平相似。暴露于RLG后,通过维持血糖正常水平,线粒体对RLG的适应性部分恢复。
综上所述,这些数据表明,HPA线粒体在RLG后发生改变,代谢转向增加脂肪酸氧化,提示神经胶质对RLG的适应包括线粒体代谢的改变,而这可能导致糖尿病低血糖的葡萄糖反调节缺陷。
原始出处:
Paul G. Weightman Potter, Julia M. Vlachaki Walker, Basal
fatty acid oxidation increases after recurrent low glucose in human primary
astrocytes
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BET#
19
#DIA#
29
#原发性#
21
#星形胶质细胞#
26
#胶质细胞#
26