Movement disorders:边缘系统5-羟色胺能可塑性,有助于改善帕金森病的淡漠状态
2022-03-12 Freeman MedSci原创
诊断时患有冷漠症的患者在诊断后5年内表现出边缘5-羟色胺神经支配的补偿性变化
帕金森病(PD)的血清素能病变与整个病程中的运动和非运动症状密切相关,根据死后组织病理学分期,血清素能病变可能早于黑质多巴胺能投射的消失。重要的是,5-羟色胺能的病理变化与早期的神经精神障碍有关,包括诊断时的冷漠、疲劳、抑郁和焦虑,但也被怀疑受到补偿性变化的影响。此外,PD的病理发展可能遵循不同的 "路线",涉及特定的单胺能功能障碍,这可能确定了以早期独特症状为特征的预后亚型。
 然而,早期PD体内5-羟色胺能病理的纵向演变及其与症状和多巴胺能病理进展的关系仍不清楚。
然而,早期PD体内5-羟色胺能病理的纵向演变及其与症状和多巴胺能病理进展的关系仍不清楚。
以前研究证明,新诊断的未治疗的(de novo)帕金森病患者伴有冷漠、抑郁和焦虑,与无神经精神症状的患者相比,他们有突出的血清能功能障碍,与内侧边缘皮质-纹状体-苍白球-丘脑回路的早期和特殊微结构改变有关,而黑质多巴胺能变性是相似的。
特别是,除了中脑白质重组外,尾状核头部和前扣带皮层的微观结构混乱和5-羟色胺能终端的功能障碍也是共同存在的。
这些发现确定了源自正中和背侧剑突状核的长程血清素能投射的早期变化,与其他研究表明PD和快速眼动(REM)睡眠行为障碍患者的早期血清素能功能障碍相一致。
此外,在晚期非痴呆患者中,合并PD的冷漠、抑郁和焦虑与中枢皮质肢体系统的多巴胺能失调有关,并被概念化为低多巴胺能行为,对多巴胺替代疗法有反应。
总的来说,怀疑帕金森病的冷漠、抑郁和焦虑有不同的病理生理基础,这取决于PD的阶段和边缘单胺能和胆碱能回路的相继功能障碍。
此外,在诊断时,无精打采的患者有更大的非运动负担和更低的认知表现,甚至在前两年持续无精打采的患者中也是如此。此外,冷漠可能预示着晚期患者的痴呆,正如在阿尔茨海默病和多发性硬化症。
然而,到目前为止,在帕金森病的早期,冷漠的长期预后意义尚不清楚。
因此,法国里昂国家科学研究中心的Stéphane Prange,等人,在诊断时有或没有冷漠症的新帕金森病患者群中,比较运动障碍和非运动神经精神症状的纵向演变,并与抑郁和焦虑症状的相关性。
核心假设:诊断时,无痛症患者和非无痛症患者在诊断后的5年内有不同的神经精神症状和血清素能病变的发展,并可能表现出边缘血清素能系统的可塑性变化。
在一项纵向的双踪迹正电子发射断层扫描队列研究中,他们招募了13名新的嗜睡和非13嗜睡PD患者。并使用[11C]PE2I检测多巴胺转运体和[11C]DASB检测血清素转运体,在基线和3至5年后量化突触前多巴胺能和血清素能病变的进展,使用线性混合效应模型和中介分析来比较各组间临床损害的纵向演变和基于兴趣区域的分析。
他们发现:开始多巴胺替代疗法后,诊断时有冷漠症的患者(n = 10)在随访时冷漠症、抑郁症和焦虑症得到改善,达到无冷漠症患者(n = 11)的水平。
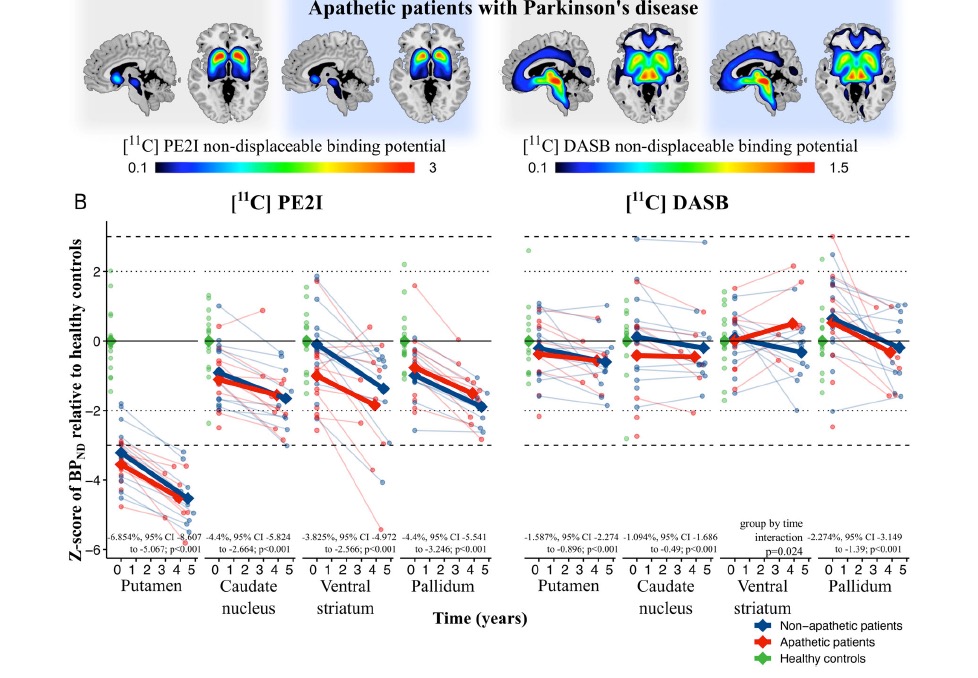
患者的运动障碍进展相似,而两组患者都出现了轻微的冲动行为。
两组患者的纹状体和中皮层突触前多巴胺能丧失的进展相似.
尾状核和苍白球的5-羟色胺能病变也是如此。相反,在冷漠症患者中,腹侧纹状体和前扣带皮层的5-羟色胺能神经支配选择性地增加,有助于在多巴胺替代疗法之外逆转冷漠症的情况。
该研究的重要意义在于发现了:诊断时患有冷漠症的患者在诊断后5年内表现出边缘5-羟色胺神经支配的补偿性变化,有希望的证据表明5-羟色胺可塑性有助于冷漠症的逆转。血清素能可塑性与多巴胺能治疗之间的关系值得进一步研究。
原文出处:
[Prange S, Metereau E, Maillet A, et al. Limbic Serotonergic Plasticity Contributes to the Compensation of Apathy in Early Parkinson’s Disease. Movement Disorders. Published online March 3, 2022:mds.28971. doi:10.1002/mds.28971](https://doi.org/10.1002/mds.28971)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Dis#
54
#disorder#
42
#ERS#
41
#disorders#
42
#Disord#
46