Cerebral Cortex:皮质-基底节区通路动态变化可能是帕金森病治疗关键
2022-03-02 影像小生 MedSci原创
PD患者运动启动的直接通路的信息流大量减少,无法释放运动,导致运动障碍/运动迟缓。通过直接路径恢复信息流可以恢复自愿运动的执行
帕金森病(PD)是一种神经退行性疾病,约1%的60岁以上人群受其影响。帕金森病是由基底神经节黑质致密部(SNc)的多巴胺能神经元进行性缺失引起的,以运动和非运动症状为特征,如运动迟缓、强直、震颤、认知障碍、抑郁和自主神经功能障碍。这些PD症状表现为多巴胺缺乏引起的基底节区功能障碍
为了阐明帕金森病皮质-基底神经节通路的网络水平变化,Atsushi Nambu等在Cerebral Cortex杂志发表研究文章Altered Dynamic Information Flow through the Cortico-Basal Ganglia Pathways Mediates Parkinson’s Disease Symptoms,该研究为PD的病理生理学增加了新的视角:皮质-基底节区通路动态信息流的改变是PD症状发生的基本病理生理学机制,其恢复是治疗PD症状的关键机制。
该研究记录了1-甲基-4-苯基-1,2,3,6-四氢吡啶治疗的帕金森病猴子的神经元活动。对运动皮层施加电刺激,分别检测苍白球内部(GPi)和外部(GPe)段,基底神经节的输出核和中继核的反应。

正常和PD状态下GPi和GPe神经元的自发放电率和皮层诱发反应
在正常状态下,皮质刺激引起GPi和GPe的早期兴奋、抑制和晚期兴奋的三相反应。在PD状态下,皮质-纹状体-GPi直接途径介导的GPi的皮质诱发抑制显著减弱,而皮质-纹状体-GPe-丘脑下(STN)-GPe途径介导的GPe的晚期兴奋被延长。

L-DOPA对PD猴GPi (A-D)和GPe (E-H)神经元皮质诱发反应和自发放电率的影响。
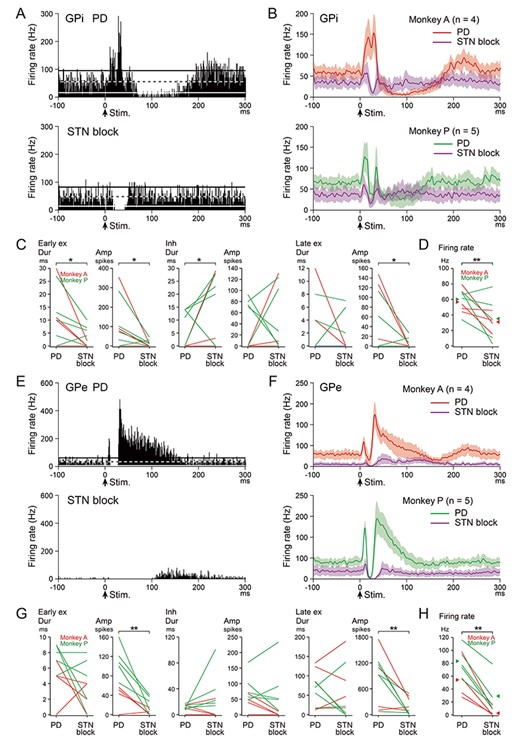
阻断STN对PD猴GPi (A-D)和GPe (E-H)神经元皮层诱发反应和自发放电率的影响。
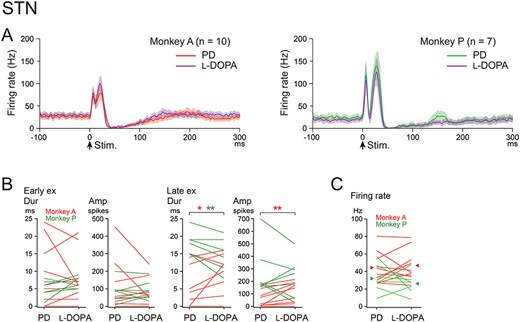
左旋多巴对帕金森病猴STN神经元皮质诱发反应和自发放电率的影响。
左旋多巴治疗改善了PD症状,特别是运动/运动迟缓,并使GPi和GPe的皮质诱发反应正常化。肌酚阻断STN可改善运动功能障碍,并可解除GPi的皮层诱发抑制。
PD患者运动启动的直接通路的信息流大量减少,无法释放运动,导致运动障碍/运动迟缓。通过直接路径恢复信息流可以恢复自愿运动的执行。
原文出处Satomi Chiken, Masahiko Takada, Atsushi Nambu, Altered Dynamic Information Flow through the Cortico-Basal Ganglia Pathways Mediates Parkinson’s Disease Symptoms, Cerebral Cortex, Volume 31, Issue 12, December 2021, Pages 5363–5380, https://doi.org/10.1093/cercor/bhab164
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#cerebral#
41
#动态变化#
27
#基底节#
0