原发性输尿管淋巴瘤1例
2019-03-17 高永华 李巧娥 马伟 医学影像学杂志
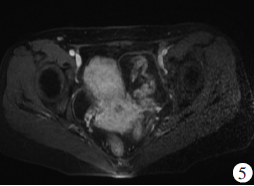
患者,男,66岁。主因进行性排尿困难2个月入院。2月前无明显原因出现排尿不畅,排尿费力,迟缓断续,射程缩短,尿线变细,终末呈滴沥状,排尿次数明显增加,每日排尿次数大于10次,近日上述症状明显加重。查体:双肾区无隆起,无压痛,无叩击痛。双侧输尿管区未见异常,膀胱无充盈,膀胱区无压痛,阴囊阴茎未见异常。肛诊:前列腺大,质韧,中间沟消失。化验:血常规、肝肾功未见异常,尿常规OB。门诊以“前列腺增生”收

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#输尿管#
46
#原发性#
31
谢谢了,学习
0
继续努力学习
70
学习了很有用不错
58
了解一下,谢谢分享!
61